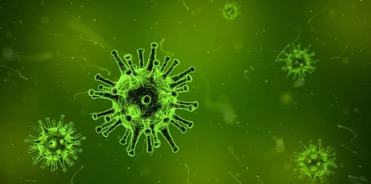
Figure 1: Researchers have identified crucial molecules utilized by the coronavirus to infect cells. With further testing, there may be a way to target these molecules to prevent viral growth, leading to broader treatments for future pandemics.
Source: Pixabay
As COVID-19 continues to spread throughout the world, scientists have made tremendous gains in understanding the virus. Their efforts have resulted in multiple vaccines with the potential to build herd immunity throughout the world. While this is an enormous victory, scientists have already started turning their efforts to prevent another such outbreak. These efforts are crucial since COVID-19 is not the only coronavirus that has historically afflicted humans, and it will likely not be the last (WebMD, 2020). There are currently seven coronavirus strains that threaten humans, with hundreds more circulating among animals. The coronavirus strains from animals can cross over to humans, in a so-called ‘spillover event,’ which scientists speculate may have occurred with the recent virus (NIAID, 2020). To combat the next spillover event, scientists have begun searching for a more comprehensive treatment that can be applied to various strains as opposed to the current strategy of tailoring treatments for each individual strain.
To reach this goal, scientists need to understand the underlying molecular processes that enable viral growth. Researchers from the Gladstone Institute and the Chan Zuckerberg Biohub, with the help of scientists at UC San Francisco (UCSF) and Synthego Corporation, have taken the first step by identifying crucial molecules the coronavirus utilizes to survive (Technology Networks, 2020). In their study, they infected normal human cells with either SARS-CoV-2, which causes COVID-19, or two other coronavirus strains that cause common colds. Unsurprisingly, the three viruses killed their respective cells. The scientists reasoned, as team leader Andreas Puschnik articulates, that “the few cells that could survive these infections presumably had mutations in host molecules that the viruses use to infect them or to multiply” (Technology Networks, 2020). Following this train of thought, the researchers used CRISPR, a gene-editing tool, to mutate human cells. They then determined what mutations made cells less vulnerable to the coronavirus. They found, as expected, that a mutation in the ACE2 receptor — widely known to be used by SARS-CoV-2 to infect host cells — enabled the cell to withstand the viral attack (WebMD, 2020). But more surprisingly, they discovered that mutations in genes that regulate two lipid molecules, cholesterol and phosphatidylinositol phosphate (PIP), prevented the virus from infecting the cells. These two molecules are known to play a role in viral infection because lipids are key components of both viral and cellular membranes, but they had not been tied specifically to the coronavirus until now (Mazzon and Mercer, 2014).
To further validate their findings, the researchers engineered cells that lacked the genes regulating cholesterol and PIP. When exposed to any of the three coronaviruses, the cells lacking those genes were completely protected (Technology Networks, 2020). In another trial, the team used existing compounds to offset cholesterol and PIP levels. Once again, the cells with lower levels of cholesterol and PIP possessed increased resistance to the coronavirus. These findings suggest that targeting cholesterol and PIP could be a promising treatment to combat not just one but multiple coronaviruses that may emerge now or later. Another leader of the study, Melani Ott, director of the Gladstone Institute of Virology, stated that “a few broader antiviral drugs that target host cells’ molecules would go a long way toward making us better prepared for future pandemic viruses” (Technology Networks, 2020). Although further studies would have to be conducted to determine such a treatment’s clinical viability, it has an exciting potential to diminish the effects of another COVID-19 level pandemic.
References
Mazzon, M., and Mercer, J. (2014, October). Lipid interactions during virus entry and infection. National Center for Biotechnology Information. Retrieved December 13, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265854/.
National Institute of Allergy and Infectious Diseases. (2020, May 19). Coronavirus. Retrieved December 13, 2020, from https://www.niaid.nih.gov/diseases-conditions/coronaviruses.
Technology Networks. (2020, December 09). Critical Molecules That Coronaviruses Hijack To Infect Human Cells Identified. Retrieved December 13, 2020, from https://www.technologynetworks.com/immunology/news/critical-molecules-that-coronaviruses-hijack-to-infect-human-cells-identified-343793.
Related Posts
How Many Humans Does it Take to Host a Planet?
Figure 1: This is an artist’s rendering of a potential...
Read MoreCOVID-19 Clinical Trials and Racial Disproportionality
Figure 1: A doctor drawing blood from a patient as...
Read MoreThe Brain and Sign Language — Evidence of a Universal Language Center?
Figure 1: The English alphabet and numbers 1-9 as signed...
Read MorePalin Narsian