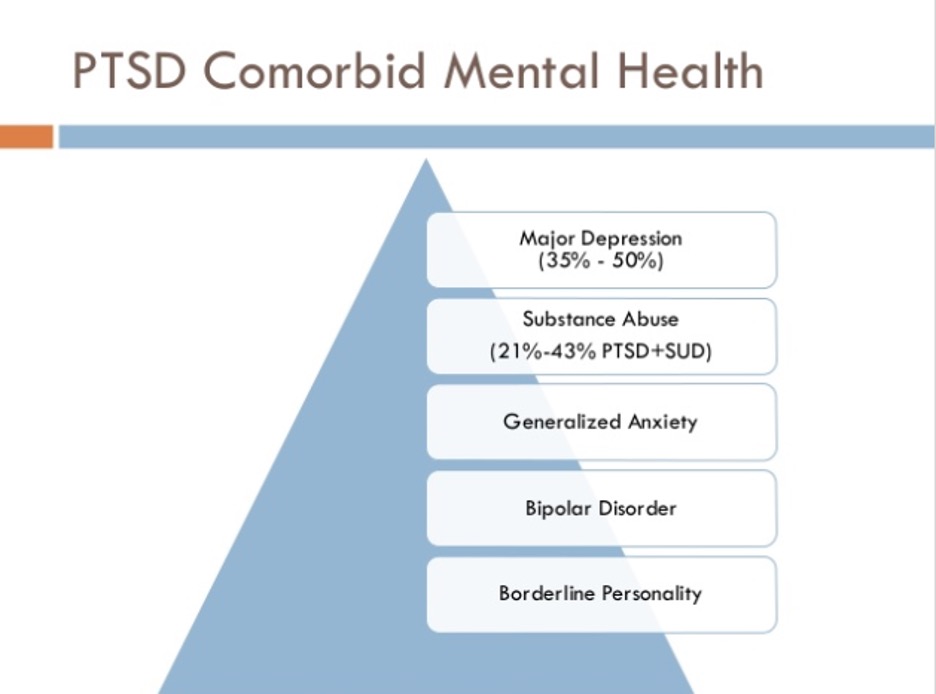
Figure 1: PTSD and its comorbid mental health symptoms contribute to the pervasive consequences of exposure to psychological trauma.
Source: Slideshare
Post-traumatic stress disorder is a pervasive and often fatal consequence of exposure to severe psychological trauma (Fenster, 2018). Epidemiological studies show that PTSD has a lifetime prevalence ranging from 1.3% to 12.2%, with variance depending on the population and sample size studied (Shalov, 2017). However, individuals with PTSD have only received an official, medical diagnosis since 1980. Since then, PTSD, and psychiatric disorders in general, have been recognized as disorders of brain circuits (Insel, 2010). Because of this relatively recent paradigm shift, large-scale genome wide association studies particular to PTSD have yet to yield significant findings. Although more time and research is needed to discover the definitive molecular changes that determine vulnerability to PTSD, emerging technologies such as optogenetics, chemogenetics, and fiber photometry have allowed for closer examination and perturbation of the macro- and microcircuits that underlie PTSD-related symptoms (American Psychiatric Association, 2007). This work provides promising opportunities for the discovery of pharmaceutical and therapeutic interventions.
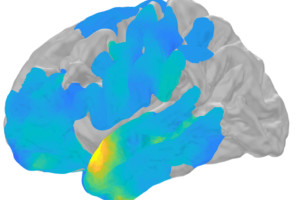
Determining effective treatments for PTSD requires understanding the disorder’s symptoms. PTSD is a leading cause of suicide and is highly comorbid with depression, other anxiety disorders, and substance abuse. Intrusion symptoms, in which the traumatic event is persistently re-experienced, perpetuate PTSD (American Psychiatric Association, 2013). The process of re-experience can occur in several ways, including recurring, involuntary intrusive memories, dissociative reactions, distressing dreams, and physiological reactivity (American Psychiatric Association, 2013). These intrusive symptoms are a product of emotional under-modulation: a failure of the cortex to inhibit the limbic system (Lanius, 2010). It is observed that individuals with PTSD have increased activity in the amygdala and decreased activity in the medial prefrontal cortex during the onset of symptoms when compared to individuals without PTSD. Individuals who have re-experiencing symptoms are also found to have increased insula activity and decreased rostral anterior cingulate cortex and inferior frontal cortex activity (Hopper, 2007). Combining these findings, it can be hypothesized that in PTSD, there is a failure of top-down cortical inhibition, meaning that the reactivation of memory traces associated with traumatic thoughts and feelings occurs despite intention to suppress them.
Intrusion symptoms are just one of many indicators associated with PTSD. Studies are also being conducted to understand the neurocircuitry effects of altered cognition and mood, symptoms that are often displayed by individuals with PTSD. Common symptoms include dissociative amnesia and memory deficits, persistent negative emotions, and altered arousal and reactivity through hypervigilance and aggressive behavior (American Psychiatric Association, 2017). More importantly, the production of brain-wide quantitative data sets will be fundamental to providing unbiased insights into how neural dynamics change in response to different cognitive demands, and how these demands are affected by stress and brain disorders. These ongoing investigations into the neurobiology of PTSD shows extreme promise for the development of feasible, neurobiology-driven approaches to treatment and prevention.
References
Fenster, R. J., Lebois, L., Ressler, K. J., & Suh, J. (2018). Brain circuit dysfunction in post-traumatic stress disorder: from mouse to man. Nature reviews. Neuroscience, 19(9), 535–551.
Shalev, A., Liberzon, I., & Marmar, C. (2017). Post-Traumatic Stress Disorder. The New England journal of medicine, 376(25), 2459–2469.
Insel, T., Cuthbert, B., Garvey, M., Heinssen, R., Pine, D. S., Quinn, K., Sanislow, C., & Wang, P. (2010). Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. The American journal of psychiatry, 167(7), 748–751.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC.
Lanius, R. A., Vermetten, E., Loewenstein, R. J., Brand, B., Schmahl, C., Bremner, J. D., & Spiegel, D. (2010). Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. The American journal of psychiatry, 167(6), 640–647.
Hopper, J. W., Frewen, P. A., van der Kolk, B. A., & Lanius, R. A. (2007). Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: symptom dimensions and emotion dysregulation in responses to script-driven trauma imagery. Journal of traumatic stress, 20(5), 713–725.
Related Posts
The Future of Wearable Devices
Figure: The colored sections of the brain represent the different...
Read MoreCOVID-19 and its Implications for Adolescent Mental Health
Covid 19 and Isolation (Source: created by author) Abstract The...
Read MoreYu Quan Ng