Figure 1:Magnetic resonance image (MRI) – coronal slice of a 4-year-old child with brain cancer. Current treatment options include standard chemotherapy, with radiation but novel nanotherapy may improve survival rates.
Source: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
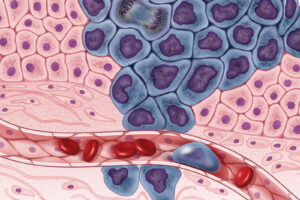
As the most common and aggressive form of brain cancer in U.S. adults, with around 14,000 new diagnoses every year, glioblastoma has been the center of significant research efforts focused on new therapeutic advances (Martin, 2019; Davis, 2016). However, even after years of advancements, the average survival of glioblastoma patients is only 12-15 months after initial diagnosis. Compared to the 12-14 months found in a separate study of treatment in the years 2000-2008, it appears as if treatment has barely advanced (Arvold & Reardon, 2014; Johnson & O’Neill, 2012). The main barrier faced by researchers in improving patient outcomes is the Blood-Brain Barrier (BBB). The BBB is a network of blood vessels that keep harmful substances out of the brain by acting as a filter. Tiny molecules such as caffeine, alcohol, and nicotine that are able to dissolve into the lipid membranes of the BBB can pass through, while larger non lipid soluble molecules cannot (Shen, 2017). Though meant to protect normal brain function, the BBB is partially responsible for the 5-year survival rate of only 5% among glioblastoma patients (Gregory et al., 2020).
Because of the complex anatomy of the brain, common surgical removal techniques of the cancerous tissue do not often yield lasting results (Venur et al., 2015). Furthermore, conventional chemotherapy drugs are unable to increase patient survival as they are blocked by the BBB, and even prior attempts to use nanoparticles for drug delivery have failed. Nanoparticles are designed to carry therapeutic particles by adjusting their size and properties to allow for more precise drug delivery (Lohcharoenkal et al., 2014). Because of these limitations, efforts towards glioblastoma treatment improvement have been largely unfruitful, until now.
A team of researchers at the University of Michigan led by Dr. Joerg Lahann and Dr. Maria Castro reported to have finally found a solution. They designed the “novel synthetic protein nano protein” (SPNP) to mimic natural proteins and viral particles already able to pass through the BBB and delivered it to patients through an IV (Gregory et al., 2020). SPNP consists of molecules like the tumor-penetrating peptide iRGD mixed with several other compounds to form a single, powerful vehicle to carry the therapeutic particles to the brain. The primary treatment molecule within the SPNP complex is an siRNA which is capable of terminating tumor growth. The peptide iRGD is responsible for chaperoning the siRNA into the brain.
In addition, given that the STAT3 pathway has been implicated in glioblastoma growth, the STAT3 inhibitor (STAT3i) is used to decrease proliferation and metastasis in order to decrease glioblastoma recurrence (Gregory et al., 2020). Though STAT3 inhibitors have been observed to have a therapeutic effect on peripheral tumors, its inability to cross the BBB alone has prevented the development of brain tumor therapies that affect the STAT3 pathway.
Another key to BBB passage is the addition of serum albumin, a compound already present in blood. The serum albumin acts much like a boat in this case, taking its therapeutic passengers (iRGD, siRNA, and STAT3i) for a ride from the outside of the BBB to inside the brain. When attempted in-vivo with mice models, in addition to existing radiation therapy, the SPNP treatment led to the long-term survival (a 45% increase of the survival period for non-treated mice) of seven out of eight mice after tumor recurrence (Gregory et al., 2020). This feat has encouraged researchers to begin designing possible clinical trials for the treatment to be initiated soon.
As the first intravenous drug delivery system to successfully pass through the BBB, the future therapeutic possibilities for brain-related disorders are immense. The SPNP can be adapted to mediate the delivery of a variety of different drugs to combat solid tumors and can provide a platform of delivery for other therapies previously hindered by the BBB. This SPNP system not only provides hope to previously forlorn glioblastoma patients, but also may serve as a blueprint for many brain-related therapies to come.
References
Arvold, N. D., & Reardon, D. A. (2014). Treatment options and outcomes for glioblastoma in the elderly patient. Clinical interventions in aging, 9, 357–367. https://doi.org/10.2147/CIA.S44259
Davis M. E. (2016). Glioblastoma: Overview of Disease and Treatment. Clinical journal of oncology nursing, 20(5 Suppl), S2–S8. https://doi.org/10.1188/16.CJON.S1.2-8
Gregory, J.V., Kadiyala, P., Doherty, R., Cadena, M., Habeel, S., Ruoslahti, E., Lowenstein, P., Castro, M., Lahann, J. (2020, November 10). Systemic brain tumor delivery of synthetic protein nanoparticles for glioblastoma therapy. Nature Communications, 11(5687) https://doi.org/10.1038/s41467-020-19225-7
Johnson, D. R., & O’Neill, B. P. (2012). Glioblastoma survival in the United States before and during the temozolomide era. Journal of neuro-oncology, 107(2), 359–364. https://doi.org/10.1007/s11060-011-0749-4
Lohcharoenkal W., Wang L., Chen Y.C., Rojanasakul Y. (2014). Protein Nanoparticles as Drug Delivery Carriers for Cancer Therapy. BioMed Research International. https://doi.org/10.1155/2014/180549
Martin, L. (2019, December 17). Glioblastoma (Primary & Secondary): Symptoms, Treatments, Diagnosis. Retrieved from https://www.webmd.com/cancer/brain-cancer/what-is-glioblastoma
Shen, H. H. (2017). Core Concept: Circumventing the blood–brain barrier. Proceedings of the National Academy of Sciences, 114(43), 11261-11263. doi:10.1073/pnas.1716187114
Venur V.A., Peereboom D.M., Ahluwalia M.S. (2015) Current Medical Treatment of Glioblastoma. In: Raizer J., Parsa A. (eds) Current Understanding and Treatment of Gliomas. Cancer Treatment and Research, 163. https://doi.org/10.1007/978-3-319-12048-5_7
Related Posts
Overview, History, Essential Concepts, and Current Topics in Transplant Immunology
First Author: Anahita Kodali1 Co-Authors: Vaishavi Agrawal2, Vivek Babu3, Sakeena...
Read MoreSingle Cell RNA Sequencing Enhances Understanding of Tumor Genetic Diversity
Figure 1: Researchers have shown that tumor cells are a...
Read MoreThe Chernobyl Accident — A Natural Experiment for the Effects of Radiation on Humans
Figure 1: A monument (front left) to the meltdown at...
Read MoreJaitri Joshi