Figure 1: The author (14 hours and 10 patients into a 16-hour shift) killing time until his next resuscitation with an issue of Prehospital Emergency Care
A car drifts across a double yellow line and slams into an oncoming tractor trailer. A man collapses on the floor of a supermarket aisle after his heart suddenly stops beating. A child gasps for breath and begins to turn blue in her mother’s arms as her airway swells in the parking lot of an ice cream parlor. In each of these cases, after emergency medical services (EMS) are activated by a 911 call, emergency medical technicians (EMTs) jump into ambulances and speed to the scene of these emergencies – major trauma, cardiac arrest, and anaphylaxis, respectively – ready to treat and stabilize critically ill patients.
As an undergraduate and EMT-B fresh out of class, I quickly realized that there are a wealth of issues in the field of prehospital care that need to be addressed in an evidence-based manner. Thankfully, I found a wonderful mentor in my university’s Department of Emergency Medicine who steered me in the direction of the right questions and introduced me to methods that can be used to pursue the relevant answers. However, I am also aware that many undergraduates are not as fortunate as I have been in this regard. To create change in any field of medicine, it is crucial to 1) have an understanding of the current standard of care treatments provided to a given class of patients 2) develop a physiologically justified question that is answerable using available or collectible data, and 3) obtain an answer that has the potential to improve patient care. With this article, I hope to be of service by briefly outlining of the role of EMS, providing an example of important research conducted in the field during the past decade, and giving the reader thirty questions that have answers with the potential to save lives and shape the future of emergency medicine.
Prehospital care has come a very long way since the beginning of EMS in the United States during the mid-20th century (Shah, 2006). What started as a system defined by throwing dying patients into repurposed hearses and then racing at high speeds to the nearest emergency room has evolved into a nationwide network of ground and air vehicles stocked with state-of-the-art equipment ranging from electrocardiograms used to analyze the heart’s electrical rhythm to portable ventilators that breathe for patients who can no longer do so on their own. This system is staffed by healthcare providers rigorously trained to perform lifesaving medical interventions that include chest compressions, defibrillation, hemorrhage control, and the proper administration of pharmacologic agents. The actions of EMTs have benefitted millions of patients who would not have survived transport to the nearest hospital without the application of immediate medical intervention.
It is indisputable that prehospital emergency care is a vital part of the healthcare system, particularly for the patients suffering from life-threatening illness for which morbidity and mortality has a time-dependent effect. Out-of-hospital cardiac arrest (OHCA) provides one striking example – for every minute following pulselessness that passes without intervention, the probability of surviving decreases by approximately 10%. For this reason, until about sixty years ago, every OHCA victim died where they fell. Then, after the development of portable defibrillators and cardiopulmonary resuscitation (CPR) in the 1960s and the movement of this technology into the prehospital setting, patients began having a chance to survive. Now, approximately 10% of cardiac arrest victims in the US survive to hospital discharge after treatment in the prehospital setting (Virani et al., 2020). While infinitely better than the 0% seen previously, it is still a sobering statistic that has seen little improvement over the past decade.
Despite this, there is hope for these patients thanks to the resuscitation researchers diligently working toward revolutionizing the standard of care we can offer these patients in the prehospital setting. One of the biggest advances in the past decade was memorably inspired by a case study of bystander CPR performed with a toilet plunger (Lurie, Lindo, & Chin, 1990). This report (in part) motivated a group of physician-scientists to conduct laboratory research that demonstrated the value of intrathoracic and intracranial pressure (ICP) modulation to improve the success of cardiac arrest resuscitation. They found that keeping pressure in the thorax low during CPR (by, for example, pulling on the chest wall during the upstroke of each compression with a suction cup/plunger to increase the volume of the thoracic cavity) is important because it maximizes the return of blood to the heart between chest compressions. Think of the heart as an untied balloon — if it is only one-quarter full, a squeeze will push much less air out (and with much less noise) than if the balloon is full of air when you begin to apply pressure. Therefore, maximizing blood return to the heart between compressions allows for more forward blood flow and better tissue perfusion. It is also important to keep ICP low during resuscitation because high ICP resists the movement of oxygenated blood from the pulmonary circuit to the brain. If oxygenated blood is not effectively reaching the brain, this will worsen post-resuscitation neurological injury.
These findings led to the development of the ResQPOD impedance threshold device (ITD) and the ResQPUMP active compression-decompression CPR device. The ResQPOD is basically a one-way valve. Once an artificial airway has been established in a cardiac arrest patient (via an endotracheal tube, which is a plastic tube inserted into the trachea, or a supraglottic airway, which is a device that seals around the anatomy above the trachea) the ITD is attached to the end of the airway. The valve allows air to be forced out of the patient’s lungs during CPR, but does not allow air back into the chest between chest compressions, which keeps the intrathoracic pressure low and increases the return of blood to the heart. (Note: Ventilations can still be delivered through the device and into the patient’s lungs, but the volume of air delivered is quicky expelled.) The ResQPUMP is essentially a suction cup with a handle attached – not dissimilar to the plunger that helped inspire its development. While CPR is being delivered using this device, instead of letting the chest wall recoil after each compression, an upward (approximately 10-kilogram) force is applied to the patient’s chest wall, which expands intrathoracic volume and therefore decreases intrathoracic pressure. This device has incorporated a force gauge and metronome to monitor compression quality. Importantly, these devices work synergistically and were found to generate more neurologically intact survivors than standard care when used together in a large randomized controlled trial (Aufderheide et al., 2011).
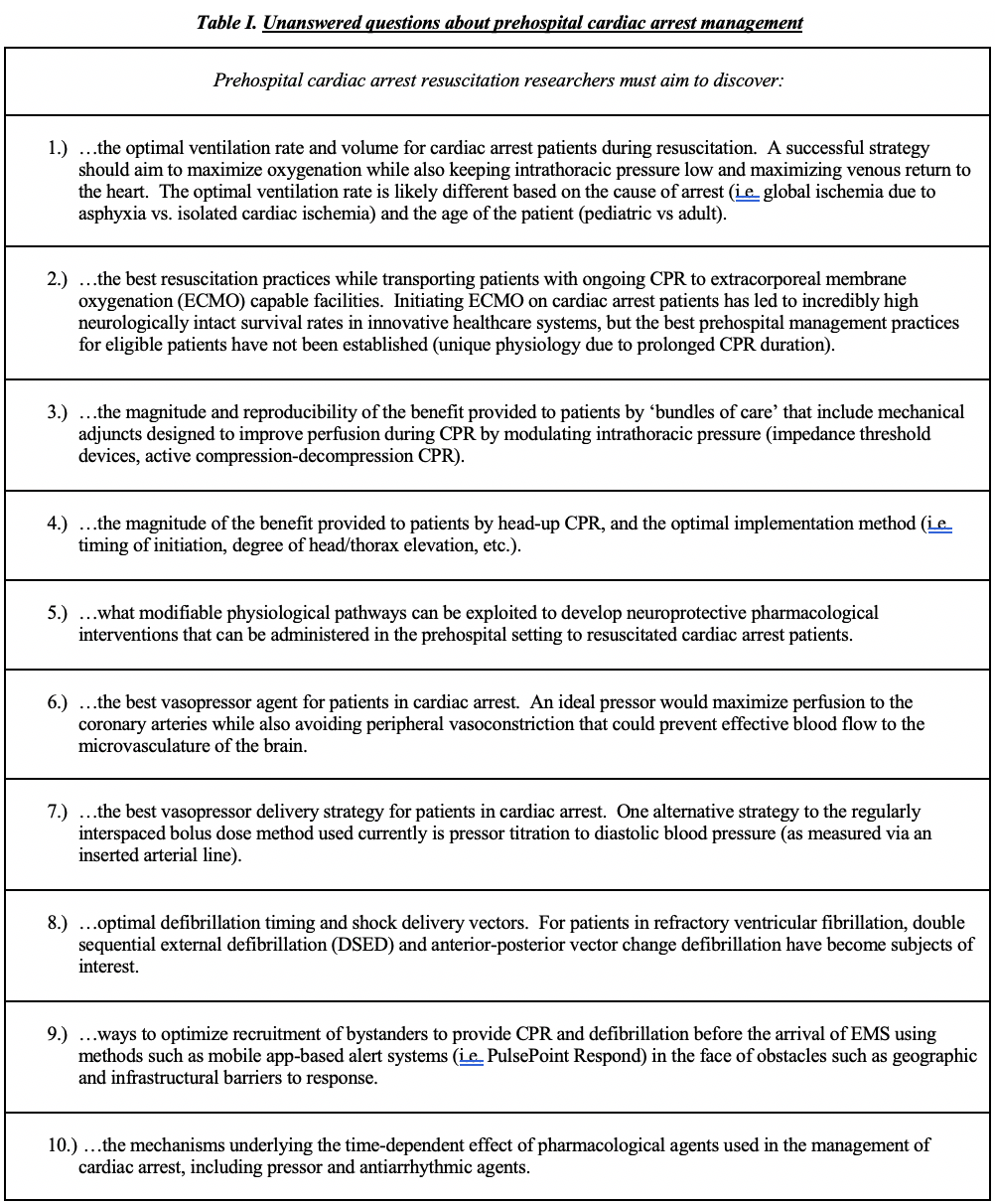
Other active areas of research include the optimization of the delivery of vasopressor and antiarrhythmic agents by prehospital providers (Daya et al., 2020; Kudenchuk, Daya, Dorian, & Resuscitation Outcomes Consortium, 2016), the development of post-arrest neuroprotective interventions (Bernard et al., 2002; Lascarrou et al., 2019), and the creation of methods to allow faster recognition of and better bystander response to cardiac arrests (Andelius et al., 2020; Blackwood et al., 2020). To quote physician-scientist Dr. Keith Lurie, we are witnessing “the dawn of a golden age of resuscitation.” Yet, there are many questions that need to be answered before definitive progress can be made, and more people need to be asking them. Examples of questions that will need to be addressed if we hope to provide the highest standard of prehospital care are provided in the following tables [Tables I, II, and III].
Cardiac arrest is only one of the many time-critical conditions that prehospital providers treat every day across the country. Massive hemorrhage, traumatic brain injury, large-vessel-occlusion stroke, and other conditions continue to cause significant morbidity and mortality that may be lessened by the evidence-based actions of EMTs. The list of medical emergencies is long, and each carries a suite of questions with potentially lifesaving answers. We still do not know the ideal methods we should be employing to treat many critical patients, and the debate is ongoing regarding a range of important topics – from the techniques employed to manage patient airways (Wang et al., 2018) to the effectiveness of some of the medications that are administered prior to hospital admission (Coats & Lecky, 2020; Kudenchuk et al., 2016; Soar, 2020).
I strongly encourage all young investigators – from undergraduates to undecided post-docs – to consider becoming involved in prehospital emergency care research. It is a rich and rewarding field with a myriad of opportunities to rapidly inform the performance of lifesaving interventions used around the world to alleviate the suffering of the sickest patients imaginable. Every moment we waste, hearts continue stopping, trauma victims continue bleeding, and lives are unnecessarily lost every minute of every day.

Glossary
Ischemia – a reduction in blood flow to tissues, which results in oxygen deprivation and the harmful accumulation of metabolic byproducts. A myocardial infarction (or ‘heart attack’) is caused by an obstruction that prevents blood from delivering oxygen to a part of the myocardium. This disease process can precipitate a sudden cardiac arrest.
Asphyxia – a state of global oxygen deprivation caused by respiratory insufficiency. If the amount of oxygen delivered to a patient’s heart is low enough for long enough, the heart will stop pumping blood. Airway obstruction and opioid overdose are two commonly encountered causes of asphyxial cardiac arrest.
Ventricular fibrillation – an abnormal cardiac electrical rhythm that does not allow the heart to pump blood effectively. Continuous, abnormal electrical discharges in the ventricles cause the cardiac muscle to ‘quiver’ instead of beating in a coordinated fashion.
Extracorporeal membrane oxygenation (ECMO) – This technique is a more advanced form of cardiopulmonary bypass. Blood is drawn out of critically ill patients, passed through a membrane oxygenator, and then returned to the body where it is able to effectively perfuse tissue.
Vasopressor – a drug given during CPR with the intention of increasing blood flow via the induction of vasoconstriction. Theoretically, decreasing the diameter of the blood vessels that contain a fixed volume of fluid will lead to increased pressure in the vascular circuit and more forward movement of blood per chest compression.
Antiarrhythmic – Drug given with the intention of preventing pathological disruptions of the heart’s normal electrical rhythm.
Resuscitative endovascular balloon occlusion of the aorta (REBOA) – this technique entails threading a balloon-tipped catheter into the femoral artery of a patient, advancing it into the aorta, and then inflating the balloon. This temporarily prevents blood flow to the lower half of the patient’s body. REBOA can be used to halt lower body hemorrhage that cannot be controlled using direct pressure or tourniquets.
PulsePoint Respond – A smartphone application that alerts users in select regions of the US to the location of cardiac arrests that occur within ~1/4 mile of their location. The app also contains a map that displays nearby AED locations. Similar pieces of software have been shown to increase the rate of bystander CPR and defibrillation prior to the arrival of EMS and improve OHCA outcomes.
References
Andelius, L., Malta Hansen, C., Lippert, F. K., Karlsson, L., Torp-Pedersen, C., Kjaer Ersboll, A., . . . Folke, F. (2020). Smartphone Activation of Citizen Responders to Facilitate Defibrillation in Out-of-Hospital Cardiac Arrest. J Am Coll Cardiol, 76(1), 43-53. doi:10.1016/j.jacc.2020.04.073
Aufderheide, T. P., Frascone, R. J., Wayne, M. A., Mahoney, B. D., Swor, R. A., Domeier, R. M., . . . Lurie, K. G. (2011). Standard cardiopulmonary resuscitation versus active compression-decompression cardiopulmonary resuscitation with augmentation of negative intrathoracic pressure for out-of-hospital cardiac arrest: a randomised trial. Lancet, 377(9762), 301-311. doi:10.1016/S0140-6736(10)62103-4
Bernard, S. A., Gray, T. W., Buist, M. D., Jones, B. M., Silvester, W., Gutteridge, G., & Smith, K. (2002). Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med, 346(8), 557-563. doi:10.1056/NEJMoa003289
Blackwood, J., Mancera, M., Bavery, S., Carbon, C., Daya, M., VanKeulen, B., . . . Rea, T. (2020). Improving response to out-of-hospital cardiac arrest: The verified responder program pilot. Resuscitation, 154, 1-6. doi:10.1016/j.resuscitation.2020.06.015
Coats, T. J., & Lecky, F. E. (2020). The CRASH3 study: prehospital TXA for every injured patient? Emerg Med J, 37(6), 392-394. doi:10.1136/emermed-2019-209264
Daya, M. R., Leroux, B. G., Dorian, P., Rea, T. D., Newgard, C. D., Morrison, L. J., . . . Resuscitation Outcomes Consortium, I. (2020). Survival After Intravenous Versus Intraosseous Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Shock-Refractory Cardiac Arrest. Circulation, 141(3), 188-198. doi:10.1161/CIRCULATIONAHA.119.042240
Kudenchuk, P. J., Daya, M., Dorian, P., & Resuscitation Outcomes Consortium, I. (2016). Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. N Engl J Med, 375(8), 802-803. doi:10.1056/NEJMc1608041
Lascarrou, J. B., Merdji, H., Le Gouge, A., Colin, G., Grillet, G., Girardie, P., . . . Group, C.-T. (2019). Targeted Temperature Management for Cardiac Arrest with Nonshockable Rhythm. N Engl J Med, 381(24), 2327-2337. doi:10.1056/NEJMoa1906661
Lurie, K. G., Lindo, C., & Chin, J. (1990). CPR: the P stands for plumber’s helper. JAMA, 264(13), 1661. doi:10.1001/jama.1990.03450130031020
Shah, M. N. (2006). The formation of the emergency medical services system. Am J Public Health, 96(3), 414-423. doi:10.2105/AJPH.2004.048793
Soar, J. (2020). Epinephrine for cardiac arrest: knowns, unknowns and controversies. Curr Opin Crit Care, 26(6), 590-595. doi:10.1097/MCC.0000000000000763
Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., . . . Stroke Statistics, S. (2020). Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation, 141(9), e139-e596. doi:10.1161/CIR.0000000000000757
Wang, H. E., Schmicker, R. H., Daya, M. R., Stephens, S. W., Idris, A. H., Carlson, J. N., . . . Nichol, G. (2018). Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA, 320(8), 769-778. doi:10.1001/jama.2018.7044
Related Posts
New ‘Drugless’ Approach to Killing Cancer Cells Shows Promise
Figure 1: Abstract Molecular Model Source: ShutterStock Researchers at Nanyang...
Read MoreTrust: The Essence of Good Policy Implementation
Figure 1 President Tsai Ing-wen inspects the Central Epidemic Command...
Read MoreThe Immunological and Physiological Effects of SARS-COV-2 on the Human Body
Figure 1: The representation of cellular activity of SARS-COV-2 as...
Read MoreTanner Smida