Figure 1: PANDAS, characterized by acute neurological and neuropsychiatric symptoms, was systematically reviewed by Sigra et al (2018) in hopes of encouraging further investigation towards the etiology and treatments associated with PANDAS and related disorders
Source: Flickr
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS), pediatric acute-onset neuropsychiatric syndrome (PANS), childhood acute neuropsychiatric symptoms (CANS), and pediatric infection-triggered autoimmune neuropsychiatric disorders (PITAND) are all characterized by episodic neuropsychiatric or neurological symptoms and thought to be attributed to aberrations within one’s immune system (Swedo et al., 1998; Allen et al., 1995; Singer et al., 2012; Swedo et al., 2012). These disorders are characterized by an acute onset––usually within 2-3 days of a trigger, whether it be streptococcal or not––of these neuropsychiatric symptoms. Patients with these conditions may also suffer from irritability, anxiety, loss of cognitive and motor ability, and uncontrollable emotions. The cause of PANS is unknown in most cases but is thought to be triggered by infections, metabolic disturbances, and other inflammatory reactions.
The first 50 cases of PANDAS were classified by Swedo et al. (1998). Many of the patients presented with obsessive compulsive disorder (OCD) and tics, but reported a variety of other symptoms as well, including separation anxiety (86–92%), issues with learning at school and coping with the classroom environment (75–81%), sleep disruptions (71%), and urinary symptoms (42–81%) (Swedo et al., 2015).
These motor and behavioral abnormalities in PANDAS cases are thought to be initiated by the antibodies created against group A β-hemolytic Streptococcus (GABHS) bacteria, which are most commonly known to cause strep throat. However, these antibodies can cross-react with autoantigens within the basal ganglia, a part of the brain controlling motor movement, and cause the neuropsychiatric symptoms associated with PANDAS (Sigra et al., 2018). The etiology of the tics and OCD symptoms of PANDAS are still unknown.
Currently, there is no cure for PANDAS. However, several clinicians have managed this disorder with antibiotics (e.g., penicillin, azithromycin, cephalosporin), therapeutic plasma exchange, intravenous immunoglobulin, tonsillectomy or adenoidectomy procedures, cognitive behavioral therapy, nonsteroidal anti-inflammatory drugs, corticosteroids, selective serotonin reuptake inhibitors, or various complementary or alternative medical treatments (Sigra et al., 2018). These interventions remain inconclusive in their efficacy, and the insufficiencies in evidence provide a weak foundation to suggest various treatments towards PANDAS and any related disorders. Thus, it is essential that further research be conducted to find the most effective regimen of PANDAS-related treatments.
With the rise of personalized medicine, it is possible that PANDAS and affiliated disorders may not have a general “cure,” but rather should be treated on a case-by-case basis. PANDAS effectively portrays the autoreactive potential of an immune response, and the off-target repercussions it may have. Ultimately further understanding the mechanisms of PANDAS, which have still yet to be discovered, will be a step in the right direction in better diagnosis and treatment of this and related conditions.
References
Allen, A. J., Leonard, H. L., & Swedo, S. E. (2010). Case Study: A New Infection-Triggered, Autoimmune Subtype of Pediatric OCD and Tourette’s Syndrome. Journal of the American Academy of Child & Adolescent Psychiatry. https://www.sciencedirect.com/science/article/pii/S0890856709637898.
Swedo, S. (2012). From Research Subgroup to Clinical Syndrome: Modifying the PANDAS Criteria to Describe PANS (Pediatric Acute-onset Neuropsychiatric Syndrome). Pediatrics & Therapeutics, 02(02). https://doi.org/10.4172/2161-0665.1000113
Sigra, S., Hesselmark, E., & Bejerot, S. (2018). Treatment of PANDAS and PANS: a systematic review. Neuroscience & Biobehavioral Reviews. https://www.sciencedirect.com/science/article/pii/S0149763417305833?via%3Dihub.
Singer, H. S., Gilbert, D. L., Wolf, D. S., Mink, J. W., & Kurlan, R. (2011). Moving from PANDAS to CANS. https://doi.org/10.1016/j.jpeds.2011.11.040.
Swedo, S. E., Leonard, H. L., Garvey, M., Mittleman, B., Allen, A. J., Perlmutter, S., … Perlmutter, S.(1998). Pediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections: Clinical Description of the First 50 Cases. American Journal of Psychiatry. https://ajp.psychiatryonline.org/doi/abs/10.1176/ajp.155.2.264.
Swedo, S. E., Seidlitz, J., Kovacevic, M., Latimer, M. E., Hommer, R., Lougee, L., & Grant, P. (2015). Clinical presentation of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections in research and community settings. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4340334/.
Related Posts
Brain Computer Interfaces: Approaches to Scientific Innovation
For more related news, check out the UnknownNow, an organization for neuroscience...
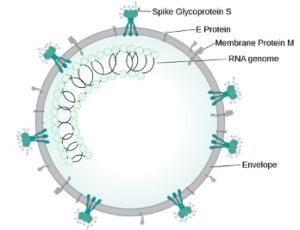
Read MoreStudy offers explanation to the COVID-19 effects on the brain
Figure 1: This is an image showing the main parts...
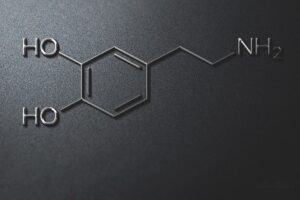
Read MoreDopamine Deficiency and Its Effects on Addiction
This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023...
Read MoreBrandon Yu