This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023 Summer Program.
With a family member who has suffered from severe ADHD as a cause of dopamine deficiency, and a lifelong struggle with obesity, I saw from a young age the importance of addressing addiction as a result of dopamine deficiency. This blog post aims to cover the connection between dopamine deficiency and addiction to food and drugs.
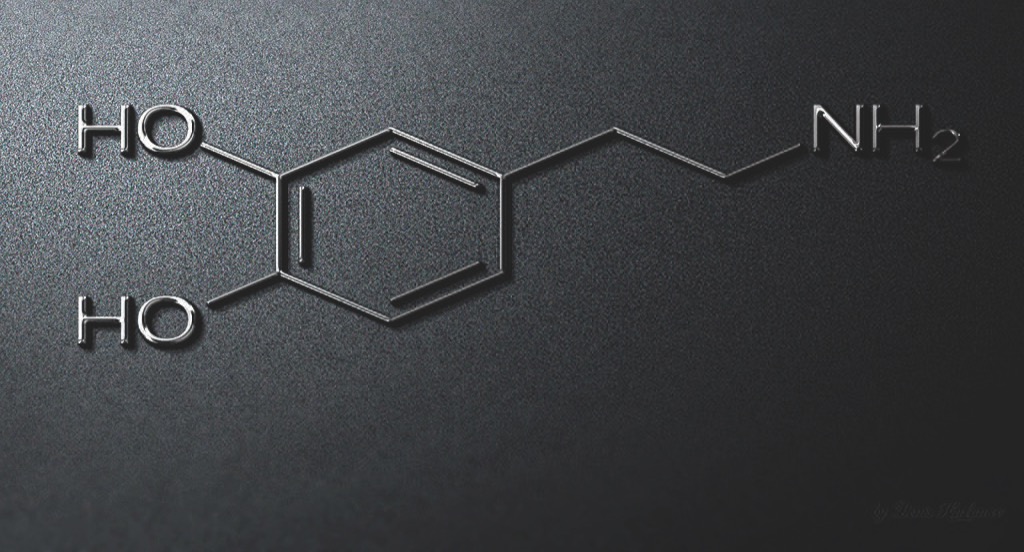
Commonly described as the “reward neurotransmitter” of the brain, dopamine is a neurotransmitter that helps relay electrochemical messages through the brain and to the rest of the body. Produced in the ventral tegmental area of the brain, dopamine is released into the nucleus accumbens and prefrontal cortex, allowing for signals triggering control of movement, memory, mood, pleasure, and cognitive abilities1. Low amounts of dopamine have detrimental effects on the body. Dopamine depletion can be caused by brain injury or hereditary conditions and is associated with widespread health problems such as obesity and drug addiction. Dopamine plays a fundamental role in satisfaction, pleasure, and happiness, and those who lack it seek these feelings from actions that produce positive sensations2. These behaviors often lead to a dependence on food or drugs for pleasure, and ultimately, addiction. The rest of the blog will dive into the correlations between dopamine deficiency and addiction.
Irregular dopamine caused by drug abuse and addiction can lead to behaviors that create a reliance on addictive substances. Dopamine is released in the mesolimbic pathway. Drugs act on this pathway, increasing dopamine transmission and damaging the pathway, creating an insatiable and ever-escalating need for the “euphoric” feeling3. With drug-related deaths nearing one million annually, over a hundred thousand in the US last year, the urgency of action against this epidemic is at an all-time high4. And of the 100,000 individuals who died due to drug overdose in 2021, 80,000 of these deaths were caused by opioids. Opioids are drugs so accessible that while 93% of insurance plans cover opioids in the US with no restrictions, the drug buprenorphine – commonly used to treat opioid addiction – is included in only 35% of insurance plans in the US without restriction5. Individuals deficient in dopamine are more likely to seek out these drugs as a counterfeit accelerator of the release of dopamine within the reward system. This allows for opioids to create a chemical imbalance in their brain and cause the lack of self-control that many addicts display.
Food addiction, while seemingly less urgent than drug addiction, affects many in the United States. With 41.9% of adults in the US facing obesity today, the issue should be treated as a national public health crisis6. Many factors play into obesity (e.g. genetics, poor sleep, environment), but a widely understudied factor that plays a large role in the rapidly growing obesity epidemic is the effects of irregular dopamine receptors in the brain, causing the heightened desire to indulge oneself and limit self-control.
The first study suggesting that food is addictive was conducted by Randolph in 1956, and from there only 9 more papers in the next 50 years were published suggesting the same. However, due to the rising concern over obesity rates in the US, and with recent breakthroughs in understanding the physiological mechanisms of obesity since the early 2000s, a boom of more than 65 papers have been produced since 20037. Some breakthroughs include studies showing that obese rats have downregulated striatal dopamine receptors similar to what is seen in drug addiction. In humans, it was found that repeated exposure to sugar induces more frequent dopamine release. Ultimately, those who have downregulated receptors are largely more susceptible to food addiction2. Another study concluded that dopamine transmitters are affected by the physiological state and access to highly palatable foods8. Often, people have a habit of eating when negative feelings arise, most notably sadness, boredom, and high stress. The vulnerability to overeating is a common factor found in binge-eating disorders and is exacerbated by the accessibility of cheap, non-nutritious foods.
In both food and drug addiction, several efforts have been made to address dopamine deficiency in those affected. Harvard has recently done research on using exercise in combination with medication-aided treatment to combat addiction, showing increased abstinence rates compared
with programs that focused on medication or physical activity separately9. Treatments available for food addiction range from 12-step programs (e.g. Overeaters Anonymous, Alcoholics Anonymous), to cognitive behavioral therapy, to psychiatric intervention. To increase the success of these efforts, stigma surrounding food and drug addiction should be minimized, and an understanding built that those affected are victims that need help more than they need criticism. Once victims are treated sympathetically, they’ll be more willing to seek help without feeling guilty about needing to get care for themselves.
Food and drug addiction is a prevalent issue in the United States that needs to be addressed. Through communal support, remedies for those affected, and public awareness about the urgency of the epidemic, victims will feel less shame associated with the issues they’re dealing with. Through the experience of my loved ones and the research I’ve done for this blog post, I have seen the significance and need for change for those impacted by addiction both medically and socially.
References
- Olguín, H. J., Guzmán, D. C., García, E. H. & Mejía, G. B. (2016). The Role of Dopamine and Its Dysfunction as a Consequence of Oxidative Stress. Oxid. Med. Cell. Longev. 2016.
- Recovery, I. A. (2019). Effects of Dopamine: How Dopamine Drives Human Behavior. Into Action Recovery Centers https://www.intoactionrecovery.com/how-dopamine-drives-our behavior/.
- Mesolimbic Pathway. http://dx.doi.org/10.1016/B978-0-12-814405-3.00017-5 doi:10.1016/B978-0-12-814405-3.00017-5.
- NCDAS. (2020). NCDAS: Substance Abuse and Addiction Statistics [2023]. https:// drugabusestatistics.org/.
- Robinson, E. Opioids more accessible than addiction treatment. OHSU News https:// news.ohsu.edu/2019/02/12/insurance-rules-make-it-harder-to-treat-opioid-use-disorder.
- CDC. (2023). HOP 2023. Centers for Disease Control and Prevention https://www.cdc.gov/ nccdphp/dnpao/state-local-programs/fundingopp/2023/hop.html.
- Lampert, C. & Novelle, M. (2023). Editorial: Neurobiology of food addiction. Frontiers in Behavioral Neuroscience. 17:1285557. doi:10.3389/fnbeh.2023.1285557
- Wallace, C. & Fordahl, S. (2022). Obesity and dietary fat influence dopamine neurotransmission: exploring the convergence of metabolic state, physiological stress, and inflammation on dopaminergic control of food intake. Nutrition Research Reviews. 35(2):236-251. doi:10.1017/S0954422421000196
- Twark, C. (2018). Can exercise help conquer addiction? Harvard Health https:// www.health.harvard.edu/blog/can-exercise-help-conquer-addiction-2018122615641.
Related Posts
Early Childhood Adversity Impacts Impulsive Decision-Making
Cover Image: An image of a girl holding a stuffed...
Read MoreCOVID-19 and its Implications for Adolescent Mental Health
Covid 19 and Isolation (Source: created by author) Abstract The...
Read MoreAccording to New Research, Blue Whale Migrations Can Be Studied Through Song
Figure 1: A blue whale’s fluke (tail fin) sticks out...
Read MoreHow the Bystander Effect on Security Robots can Hamper Law Enforcement
BigDog robots being tested under the supervision of a Boston...
Read MoreThe E.C.H.O. Initiative: Encouraging Cardiovascular Health Through Outreach
This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023...
Read MoreThe Geography of Disease: a Bayesian Approach to Epidemiology
Figure 1: A map showing relative rates of pancreatic cancer...
Read MoreEmma Bai






