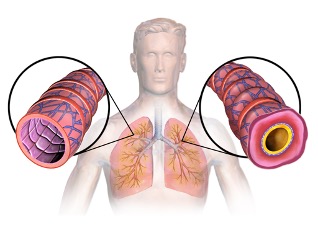
Figure 1: This diagram displays the results of tissue remodeling in the lungs. The smooth muscle along the airway appears to be swollen, and is much thicker than that in healthy, functional lungs
Source: Wikimedia Commons
Asthmatics often recount their episodes as feeling like their lungs are constricted or that their throat is tight. This sensation is due to fibrosis and tissue remodeling, two issues at the root of most of the common symptoms of asthma (Herro et al., 2020). Fibrosis and tissue remodeling occur when tissue builds up along the airway as a reaction to trauma. The restructured area has tougher cells and an abundance of “sticky” proteins (such as collagen) created by fibroblasts. This build up inhibits the airway’s ability to stretch when the lungs fill with air, creating the squeezing feeling commonly connected to asthma (La Jolla Institute for Immunology, 2020).
For many years, the causes of asthma have been widely unknown, although it was understood that some symptoms of asthma arise due to environmental and genetic factors (What Causes Asthma?, n.d.). As a result, treatments for asthma have been aimed at the symptoms of asthma rather than the cause (Royce et al., 2012). This is problematic because in cases of severe asthma, the symptoms may appear rapidly, and if they are not treated immediately, can lead to dangerous outcomes. It therefore would serve patients well to be preventative in treating asthma rather than reactive.
Researchers have been working to achieve a more thorough understanding of fibrosis and tissue remodeling to treat diseases such as asthma more effectively. Recently, a protein called TL1A, a known co-stimulatory factor in the inflammatory response, was identified as a potential contributor to fibrosis in the lungs. In mouse models, inhibition of the TL1A-DR3 pathway directly reduced lung inflammation (Hsu & Viney, 2011).
Further studies show that TL1A interacts with the DR3 receptor on cells in the lungs and bronchial tubes to stimulate fibroblasts to create collagen and other “sticky” proteins. TL1A also contributes to tissue remodeling by signaling for fibroblasts to coat the preexisting smooth muscle along the airway to form the build-up that stiffens the airway (La Jolla Institute for Immunology, 2020). What’s more, patients with severe asthma have been found to have more TL1A than patients without asthma, further cementing TL1A’s involvement (La Jolla Institute for Immunology, 2020).
Given all this, a treatment for asthma aimed at suppressing the TL1A-DR3 pathway could be revolutionary. Such a treatment could address both fibrosis and tissue remodeling simultaneously while eliminating the danger of experiencing the symptoms of asthma almost entirely. However, since TL1A is involved in inflammatory response mechanisms throughout the body, some of them important to normal immune function, there is the potential for dangerous side effects in the event that the medication is found to be even marginally non-specific. Much more research is still needed, but even so, the potential for TL1A protein-based therapy is exciting.
References
Herro, R., Miki, H., Sethi, G. S., Mills, D., Mehta, A. K., Nguyen, X.-X., Feghali-Bostwick, C., Miller, M., Broide, D. H., Soloff, R., & Croft, M. (2020). TL1A Promotes Lung Tissue Fibrosis and Airway Remodeling. The Journal of Immunology, 205(9), 2414–2422. https://doi.org/10.4049/jimmunol.2000665
Hsu, H., & Viney, J. L. (2011). The tale of TL1A in inflammation. Mucosal Immunology, 4(4), 368–370. https://doi.org/10.1038/mi.2011.20
La Jolla Institute for Immunology. (2020, September 25). A step toward helping patients breathe deeply: Scientists track down a protein that may add to lung damage in asthma and related diseases. https://www.sciencedaily.com/releases/2020/09/200925113630.htm
Royce, S. G., Cheng, V., Samuel, C. S., & Tang, M. L. K. (2012). The regulation of fibrosis in airway remodeling in asthma. Molecular and Cellular Endocrinology, 351(2), 167–175. https://doi.org/10.1016/j.mce.2012.01.007
What Causes Asthma? (n.d.). Retrieved December 21, 2020, from /lung-health-diseases/lung-disease-lookup/asthma/asthma-symptoms-causes-risk-factors/what-causes-asthma
Related Posts
Bacterial Treatment of Cancer
Abstract: Cancer treatment has long been an engaging field of...
Read MoreBalancing Blood Sugar: The Evolution of Glucose Monitoring
Figure 1: Many people diagnosed with diabetes often rely on...
Read MoreThe Gut May Be The Door to Effective Depression Treatment
First Author: Jillian Troth1 Co-Authors [Alphabetical Order]: Roxanna Attar2, Caroline...
Read MoreJulia Patterson



