This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023 Summer Program.

Source: NIAID
Since the 1930s, antimicrobial resistance (AMR) has steadily been on the rise. Affecting over two million people every year1, AMR is especially devastating for low-income and underfunded communities. Families in these regions are 1.5 times more likely to die from AMR-related infections due to a lack of healthcare facilities and supplies1. This article will explore the consequences of AMR across underprivileged communities.
Antimicrobial Resistance
AMR is the ability of infectious bacteria and other pathogens in the body to become resistant to antibiotics that are used to treat them. As a result, bacteria can transform into even deadlier threats, while becoming increasingly resistant to drugs. Interestingly, AMR bacteria have become resistant to a variety of antibiotics including methicillin, (methicillin-resistant Staphylococcus aureus or staph), vancomycin, and carbapenems.
In 2014, the World Health Organization (WHO) declared AMR to be a global epidemic due to the rapid spread of resistant bacteria. Shortly after, in September 2016, the United Nations General Assembly (UNGA) declared AMR to be a global health issue1.
Repercussions of AMR in Underprivileged Populations
AMR is a serious problem in low-income areas for four main reasons: lack of access to healthcare, environmental and socio-economic disparities, insufficient education and awareness, and cultural beliefs.
- Lack of access to healthcare: In 2021, the average healthcare cost per person in the US was $12,900 per person2. In most low-income communities, healthcare facilities such as hospitals and clinics are scarce. Families who cannot afford transportation services or healthcare bills often resort to using over-the-counter (OTC) antibiotics. The constant use of these common medications, which are cheaper and easier to access, increase the chance for bacteria to develop resistance3.
- Environmental and Socioeconomic imbalances: In most low-income communities, socio-economic challenges include overcrowded housing, sanitation, and clean water. Unhygienic conditions can cause bacteria and other pathogens to spread. Environmental conditions in these places such as poor waste management and access to food containing antimicrobial-resistant bacteria also cause resistance to develop in these individuals4. AMR bacteria in animals can transfer into food and enter humans, increasing the chance for resistance5.
- Limited Healthcare Education and Awareness: Many underprivileged communities lack proper educational resources about health. As a result, many families form their own beliefs that range from distrust of doctors to self-medication, all of which contribute to bacterial resistance6. Self-medication especially increases the chances for AMR as the drugs ingested could be unsuitable for the particular illness, which can in turn strengthen AMR bacteria7.
- Cultural Beliefs: Many cultural and social beliefs about medicine also cause individuals to self-medicate or use medicine given by cultural practitioners. These medicines are not always efficient in combating infections, which means the bacteria remain and continue growing in the body. Consequently, the bacteria adapt to their surroundings to become more resistant over time. Low awareness about the proper use of antibiotics as mentioned above also contributes to this reason for AMR8.
AMR Effects on Mental Health
AMR causes prolonged illnesses and diseases which can take a toll on an individual’s mental health, especially on one living in a low-income community. AMR-based infections have been reported to increase mental disorders through direct neurotoxicity, which occurs when infectious bacteria cross the blood barrier and damage the nervous system. AMR-induced infections from an early age can also contribute to developing mental disorders9, such as anxiety and depression, as a result of bullying and health-related absenteeism from chronic AMR infections10. These mental concerns can follow individuals into adulthood, transitioning into issues such as OCD and schizophrenia9. Therefore, reducing the spread of AMR can prevent the rise of harmful illnesses both physically and mentally.
Ongoing Efforts to Combat AMR
Although AMR has been a global issue for several decades, public health interventions to mitigate and control this condition have only recently begun. In 2001, the WHO published the WHO Global Strategy for Containment of Antimicrobial Resistance, which is a framework of possible interventions necessary to slow the spread of bacterial resistance, such as legislative actions to promote better healthcare and educate communities about AMR and health. In 2014, it published data about its surveillance on the extent of the spread of AMR to better understand where AMR is the most significant and in need of reduction. Since 2012, WHO’s project CAESAR (Central Asian and Eastern European Surveillance of Antimicrobial Resistance) has sought to combat AMR by developing connections between countries worldwide, gathering information about the spread of AMR, and supporting labs in researching ways to reduce AMR1. To prevent the spread of AMR from animals to humans, the Organization for Animal Health (OIE) and the Food and Agriculture Organization of the United Nations (FAO) have produced resolutions and policies to implement as well11. The OIE has aligned with WHO on the concept of “One Health” where animals and humans are interlinked in the transfer of AMR. Their strategy includes encouraging international legislative rules for global health and improving awareness of AMR12. FAO’s action plan ensures that humans have access to safe foods and animals have safe feeds to eat from, They have adopted resolution 4/2015 which plans to through promotion of proper antimicrobial usage AMR risk communication, and animal health and safety13.
What Can We Do?
There are numerous initiatives we can take to address AMR in our communities. First, we need to focus on hygiene and sanitation, such as through hand washing14. Specifically, we can lead efforts and campaigns to provide families in low-income places with better sanitation options. Second, better medical advising for low-income communities on how to safely use medication is necessary. This can help individuals understand the health implications of non-recreational and inadequate usage of medicines which can help prevent AMR. Working to ensure that food is processed hygienically should also be a priority15.
References
Why are Americans paying more for healthcare? https://www.pgpf.org/blog/2023/01/why-are-americans-paying-more-for-healthcare.
Chronic illness in childhood linked to higher rates of mental illness. Queen Mary University of London https://www.qmul.ac.uk/media/news/2020/smd/chronic-illness-in-childhood-linked-to-higher-rates-of-mental-illness.html (2020).
OIE Strategy tackles the threat of Antimicrobial Resistance (AMR) in Animals. WOAH – World Organisation for Animal Health https://www.woah.org/en/oie-strategy-tackles-the-threat-of-antimicrobial-resistance-amr-in-animals/ (2016).
The FAO action plan on antimicrobial resistance 2021–2025. https://www.fao.org/family-farming/detail/en/c/1456387/.
AMR prevention. https://www.pfizer.com/science/focus-areas/anti-infectives/amr-prevention.
Antibiotic resistance. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance.
Related Posts
Mind Missing Out? Fear of Missing Out and the Brain
Figure: A person scrolling through news articles on their smartphone....
Read MoreAccording to New Research, Blue Whale Migrations Can Be Studied Through Song
Figure 1: A blue whale’s fluke (tail fin) sticks out...
Read MoreHow Many Humans Does it Take to Host a Planet?
Figure 1: This is an artist’s rendering of a potential...
Read MoreDancing Neurons & Their Exciting Impacts
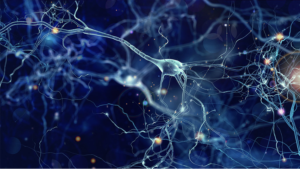
Figure 1: A network of neurons in the brain Source: Elizabeth...
Read MoreGeorge Washington Carver: “The Peanut Man”
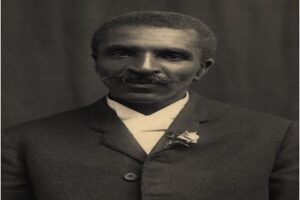
Figure 1: George Washington Carver: “The Peanut Man” (Photograph ca. 1910)...
Read MoreWhen the Going gets Tough, the Close start Nearing: Networks and External Stress
Figure: A Social Network (Wikimedia Commons, Author Zigomitros Athanasios –...
Read MoreMedha Modekurti