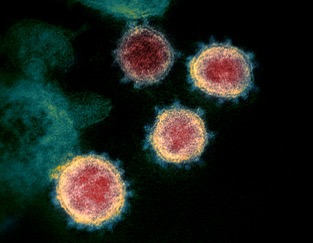
Figure 1: Transmission electron microscope image of the SARS-CoV-2 virus. The ligands on the surface of the virus bind to receptors in the olfactory bulb
Source: Wikimedia Commons
Even as researchers continue to uncover more about the SARS‐CoV‐2 virus, the long-term effects of COVID-19 remain unstudied. However, decades of past studies on similar viruses combined with recent research indicates that COVID-19 may inflict serious lasting damage to the nervous system and brain. This may include increased risk or worsening progression of Alzheimer’s Disease and other neurodegenerative diseases, as well as depression and other psychiatric disorders (Erausquin et al., 2021).
In an Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association paper published in January 2021, a group of researchers from universities across the world, led by Dr. de Erausquin, warned of the potential chronic harms inflicted on the human body by the SARS‐CoV‐2 virus behind the COVID-19 pandemic (Erausquin et al., 2021). The researchers referenced flu-like diseases spread in the past, such as those caused by viruses H1N1 and SARS-CoV, that have been strongly linked with brain disorders that affect memory and behavior. For example, studies of human brain cells indicate that one of the viruses that causes cold sores, the herpes simplex virus 1 (HSV1), correlates with cognitive decline and even pathology associated with the molecular mechanisms of dementia and Alzheimer’s Disease (Cairns et al., 2020). These correlations have served as a base for researchers to launch their investigations on SARS‐CoV‐2.
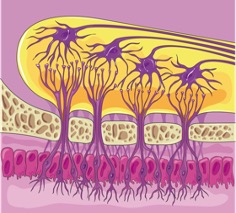
Figure 2: Olfactory bulb with its connecting neurons
Source: Wikimedia Commons
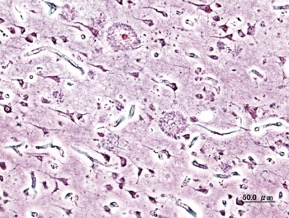
In most observed patients, common symptoms relating to the nervous system such as headaches, hypogeusia (reduced taste), and anosmia (loss of smell) appeared before respiratory symptoms (Baig, 2020). The origin of loss of smell is the olfactory bulb, in which two receptors — angiotensin-converting enzyme 2 (ACE2) and transmembrane serine protease 2 (TMPRSS2) — are found to be binding sites for SARS‐CoV-2 that aid its replication and accumulation (ACS Chemical Neuroscience, 2020). Furthermore, the olfactory bulb may be a springboard for SARS-CoV-2 to advance further into the brain all the way to the hippocampus (located in the center of the brain and responsible for short-term memory), as demonstrated by a study showing that SARS-CoV-2 administered intranasally in mice invaded the brain rapidly (Jiang et al., 2020). Recent post-mortem studies show traces of SARS‐CoV-2 in the brain while brain imaging studies reveal significant abnormal changes in COVID-19 patients, including the presence of demyelinating lesions in several brain regions and the spine (Zanin et al., 2020), even for patients whose only symptom was the loss of smell (Politi et al., 2020). When demyelination occurs, nerve impulses slow or even completely halt, leading to severe neurological problems.
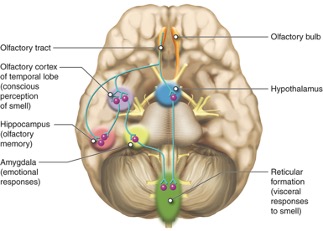
Figure 3: Olfactory bulb, the hippocampus, and other structures
Source: Lumen Learning
Additional neural symptoms, including delirium, ataxia (impaired balance or coordination), and altered mental state (Baig, 2020), might lead to cognitive decline and psychiatric shifts over time in the form of sensorimotor, mental, and behavioral disorders (Mao & Jin, 2020). Even those who are afflicted with milder infections with few symptoms are at risk for permanent damage that may severely impact quality of life (Erausquin et al., 2021).
To shed light onto the exact implications of these findings, an international consortium intending to bring results as early as 2022 will collect information on the cognition, behavior, and MRI-measured brain volumes of two groups of participants — one group of COVID-19 patients documented in hospitals around the world, and another group of participants in existing research studies. Funded by the Alzheimer’s Association with guidance from the World Health Organization, the study aims to investigate how COVID-19 may increase the risk and progression of neurodegenerative diseases and psychiatric disorders such as Alzheimer’s Disease and depression (Erausquin et al., 2021).
References
Baig, A. M. (2020). Neurological manifestations in COVID‐19 caused by SARS‐CoV‐2. CNS Neuroscience & Therapeutics, 26(5), 499–501. https://doi.org/10.1111/cns.13372
Cairns, D. M., Rouleau, N., Parker, R. N., Walsh, K. G., Gehrke, L., & Kaplan, D. L. (2020). A 3D human brain–like tissue model of herpes-induced Alzheimer’s disease. Science Advances, 6(19), eaay8828. https://doi.org/10.1126/sciadv.aay8828
Erausquin, G. A. de, Snyder, H., Carrillo, M., Hosseini, A. A., Brugha, T. S., & Seshadri, S. (2021). The chronic neuropsychiatric sequelae of COVID-19: The need for a prospective study of viral impact on brain functioning. Alzheimer’s & Dementia, n/a(n/a). https://doi.org/10.1002/alz.12255
Jiang, R.-D., Liu, M.-Q., Chen, Y., Shan, C., Zhou, Y.-W., Shen, X.-R., Li, Q., Zhang, L., Zhu, Y., Si, H.-R., Wang, Q., Min, J., Wang, X., Zhang, W., Li, B., Zhang, H.-J., Baric, R. S., Zhou, P., Yang, X.-L., & Shi, Z.-L. (2020). Pathogenesis of SARS-CoV-2 in Transgenic Mice Expressing Human Angiotensin-Converting Enzyme 2. Cell, 182(1), 50-58.e8. https://doi.org/10.1016/j.cell.2020.05.027
Journal article reviews century of data showing COVID-19 likely to impact the brain: International consortium funded by Alzheimer’s Association will study effects. ScienceDaily. (n.d.). Retrieved January 10, 2021, from https://www.sciencedaily.com/releases/2021/01/210106171340.htm
Mao, X.-Y., & Jin, W.-L. (2020). The COVID-19 Pandemic: Consideration for Brain Infection. Neuroscience, 437, 130–131. https://doi.org/10.1016/j.neuroscience.2020.04.044
Politi, L. S., Salsano, E., & Grimaldi, M. (2020). Magnetic Resonance Imaging Alteration of the Brain in a Patient With Coronavirus Disease 2019 (COVID-19) and Anosmia. JAMA Neurology, 77(8), 1028. https://doi.org/10.1001/jamaneurol.2020.2125
SARS-CoV-2: Olfaction, Brain Infection, and the Urgent Need for Clinical Samples Allowing Earlier Virus Detection | ACS Chemical Neuroscience. (n.d.). Retrieved January 10, 2021, from https://pubs.acs.org/doi/abs/10.1021/acschemneuro.0c00172
Zanin, L., Saraceno, G., Panciani, P. P., Renisi, G., Signorini, L., Migliorati, K., & Fontanella, M. M. (2020). SARS-CoV-2 can induce brain and spine demyelinating lesions. Acta Neurochirurgica, 162(7), 1491–1494. https://doi.org/10.1007/s00701-020-04374-x
Related Posts
Exploring Possibilities for the Early Diagnosis of Alzheimer’s Disease
Figure 1: Extracellular deposits of amyloid-beta proteins as seen in...
Read MoreHow Genetic Engineering Can Responsibly Revolutionize Healthcare Treatment
Source: iStock At just 3 months old, Victoria Gray was...
Read MoreWhy Do We Really Need Vitamins?
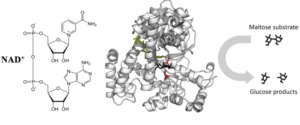
Figure 1: This figure illustrates the interaction between an enzyme,...
Read MoreMiranda Yu


Comments are closed.