Figure 1: Cell culture in a Petri dish
Source: Wikimedia Commons
Melanomas are one of the rarest but most deadly skin cancers. Just like other cancers, earlier detection often results in better prognosis due to early intervention measures like chemotherapy. Unlike other cancers, however, early detection of melanomas is often a challenge due to technical difficulties, such as DNA sequencing errors when assaying pernicious mutations that affect small cell colonies in the early stages of the disease. Because of this, accurate detection often occurs only in later stages, when the cancer is far more dangerous. In cases of late detection, post treatment five-year survival rates are 65% when the cancerous cells spread to the lymph nodes and 25% in cases of systemic propagation. (SEER, 2014).
Overexposure to the sun’s UV rays has been implicated as one of the common causative agents of skin cancer. The epidermis, being the outer layer of the skin, is chronically susceptible to mutations. In a normal state, intrinsic repair pathways exist to rejuvenate damaged skin. However, overexposure to U.V radiation can result in irreparable mutations, which can later develop into skin cancers. 90% of these mutations affect the keratinocytes (keratin producing cells), leading to cancers which are typically treatable and have a better survival prognosis (Martincorena, 2015). When mutations occur in the genes of melanocytes (melanin producing cells), however, a replication cascade results in mutant colonies that tend to form melanomas.
In a quest to understand the genesis of somatic mutations, especially in melanocytes, Tang et. al engineered a hybrid gene sequencing method that aligns two different techniques to produce more reliable data. The first technique, whole genome amplification (WGA), is invaluable in the creation of multiple copies of a genome. It involves techniques such as PCR (Polymerase Chain Reaction), which uses a heat stable synthetic DNA polymerase enzyme and a pool of oligonucleotides to make copies of DNA. The second technique, In vitro cultivation of cells into colonies, involves placing the cells in suitable mediums and allowing biological replication to occur at its own pace. In the former approach, using WGA alone, amplification introduces many errors per cell which may be confused as genuine mutations. The new method augments the error-prone WGA (Lodato, 2015) with slow but more accurate in vitro cultivation of single cells into colonies (Welch, 2012).
Using their new hybrid approach, the researchers came up with a number of interesting findings about melanoma growth. For one, they corroborated previous conclusions about melanoma producing genes that activate the MAPK signaling pathway such as BRAF and NRAS. In a twist, two of the most ubiquitous mutations in melanomas [BRAFv600E, mostly in moles, and a regulatory site in the TERT gene] were absent from many of their cell cultures. Tang and his team therefore hypothesized the existence of a spontaneous melanoma that develops de novo, without arising from mutant moles which causes 25% of melanomas (SEER, 2014).
Furthermore, data from the research also demonstrated that regions of skin with intermittent sun exposure, such as the back, have higher mutation rates than chronically exposed areas such as the face. Tang et. al speculate that this observation could help explain the bodily distribution of melanomas, although further studies on larger cohorts will be needed to affirm the discovery.
The paper derived fundamental and reliable clues on the origins of melanocyte mutations and paves the way for further research on the pathology of similar somatic mutations. Their findings create avenues for precision medicine, particularly in improving therapies targeting specific mutations (Jin, 2019). According to one of the senior authors, Hunter Shain, the genomic methods used to probe the melanomas could be repurposed and used to estimate baseline melanoma risk in the general population and to make recommendations for screening protocols. Clearly, the applications of these discoveries are very broad.
References
Blokzijl, F., De Ligt, J., Jager, M., Sasselli, V., Roerink, S., Sasaki, N., & Nijman, I. J. (2016). Tissue-specific mutation accumulation in human adult stem cells during life. Nature, 538(7624), 260-264.
Jin, J., Wu, X., Yin, J., Li, M., Shen, J., Li, J., & Cho, C. H. (2019). Identification of genetic mutations in cancer: challenge and opportunity in the new era of targeted therapy. Frontiers in oncology, 9, 263.
Lodato, M. A., Woodworth, M. B., Lee, S., Evrony, G. D., Mehta, B. K., Karger, A., & Luquette, L. J. (2015). Somatic mutation in single human neurons tracks developmental and transcriptional history. Science, 350(6256), 94-98.
Martincorena, I., Roshan, A., Gerstung, M., Ellis, P., Van Loo, P., McLaren, S., & Stebbings, L. (2015). High burden and pervasive positive selection of somatic mutations in normal human skin. Science, 348(6237), 880-886.
“SEER Stat Fact Sheets: Melanoma of the Skin”. NCI. Archived from the original on 2014-07-06.
Tang, J., Fewings, E., Chang, D., Zeng, H., Liu, S., Jorapur, A., & Arron, S. T. (2020). The genomic landscapes of individual melanocytes from human skin. Nature, 586(7830), 600-605. https://www.nature.com/articles/d41586-020-02749-9
Welch, J. S., Ley, T. J., Link, D. C., Miller, C. A., Larson, D. E., Koboldt, D. C., & Kandoth, C. (2012). The origin and evolution of mutations in acute myeloid leukemia. Cell, 150(2), 264-278.
Related Posts
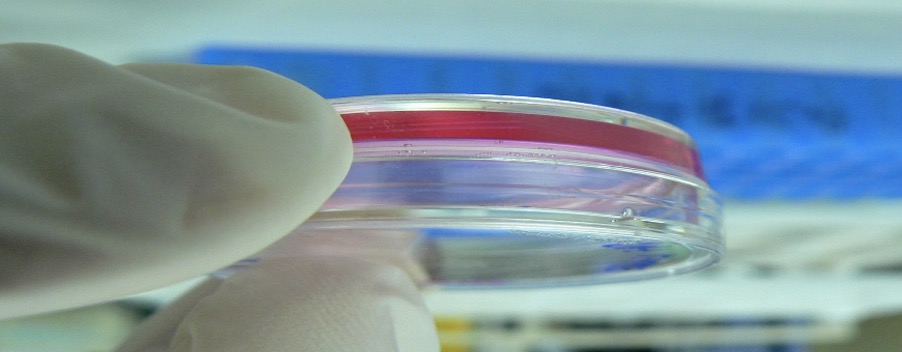
METMAP: Mapping metastatic progression
Figure 1: The start of metastasis – the movement of...
Read MoreAnother Genetic “Letter” Found in Viruses
Figure 1: A schematic of the double helix of DNA ...
Read MoreGenomic Research For All Humanity
From DNA to Life. (Source: Wikimedia Commons, William Crochot) Our...
Read MoreWhitney Nicanor Mabwi