Figure: An image of a woman wearing a mask, isolated in her home during the pandemic quarantine. (Source: Google Photos, Author: Justin Paget Getty)
Prevalent social isolation during COVID-19 lead to widespread psychological distress in the population, including the experience of loneliness, which has become increasingly recognized as a major public health issue in recent years (Cudjoe & Kotwal, 2020; Hawkley et al., 2006). A prevalence study found that more than 22% of Americans and 23% of British people have reported feeling lonely during the pandemic (Meisters et al., 2021).
Loneliness is a psychological state that has a negative impact on one’s psychological and mental health. Notably, loneliness is a subjective experience as opposed to the objective condition of social isolation (Freak-Poli et al., 2021). Loneliness, also known as perceived isolation, is characterized not only by physical isolation from social relationships, but also by negative perceptions of social interactions and connectedness, which reinforce feelings of isolation and anxiety. That is to say, loneliness is a negative situation that occurs not just as a result of an individual’s insufficient quantity of social relationships, but also, and more importantly, insufficient quality (Buecker et al., 2021). We may still feel lonely despite having a large and diverse social network, and at the same time, may rarely feel lonely when in a meaningful 1-on-1 relationship despite having a small social network. Based on these observations, researchers have defined loneliness as a discrepancy between desired and actual social connectedness (Sermat, 1984; Smoyak, 1984).
Loneliness can exert detrimental effects on mental and physiological health, resulting in worsened mental and physical symptoms, including cardiovascular disease, depression, and suicidal ideation (Gottlieb & Bergen, 2010; Killgore et al., 2020). Of note, the effects of acute loneliness are distinct from those of chronic loneliness (Shams et al., 2017). One interpretation is that chronic loneliness may function as a continuous psychological stressor which increases the allostatic load – the wear and tear resulting from chronic over-reactivity of stress systems (Clark et al., 2007). Because chronic loneliness tends to cause more serious health problems that are harder to recover from, this article will focus on chronic loneliness.
Factors influencing or triggering loneliness have been well-documented, including lack of emotional support stress, entrapment, social deficiency, low self-esteem, hopelessness, shyness, low levels of emotional intelligence, experience of trauma, lack of access to social support, and lack of access to treatment (Aust et al., 2014; Burke & Segrin, 2014; Perron et al., 2014; Zhang et al., 2014; Chang et al., 2015; Clark et al., 2015; Wols et al., 2015).
Loneliness prompts both physiological and psychological disorders. Physiologically, there is growing evidence of the association between chronic loneliness and immune system dysfunction, including reduced numbers of natural killer cell – a key cellular component of the innate immune response (Segerstrom & Miller, 2004) – and impaired immune responses to acute stressors in lonely individuals (Kennedy et al., 1988). Chronic loneliness has also been linked to elevated blood pressure (Hawkley et al., 2006; Hawkley et al., 2010) as well as an increased risk of coronary heart disease and stroke (Cacioppo et al., 2000). Moreover, feelings of social isolation are a risk factor for obesity (Gerst-Emerson & Jayawardhana, 2015) and poor sleep quality (Alsulami et al., 2019). Sleep deprivation in turn can trigger feelings of loneliness, reinforcing a self-perpetuating cycle of social withdrawal (Morneau‐Vaillancourt et al., 2021). Psychologically, perceived social isolation has been linked to higher levels of depressive symptoms (Wolf & Davis, 2014), anxiety (Käll et al., 2020), psychosocial stress (Hänsel et al., 2010), and cognitive decline in dementia and Alzheimer’s disease (Burns et al., 2022). Patients prone to substance abuse (Boyle & Davis, 2006), borderline personality disorder (Leichsenring, 2004), and schizoid personality disorder (Cavicchioli & Maffei, 2020) also reported higher levels of loneliness and social disconnection than healthy controls. Furthermore, loneliness is a risk factor for post-traumatic stress disorder (Pietrzak et al., 2021) and enhances intrusive thoughts following trauma exposure (Pan et al., 2021).
Taken together, there seems to be a bi-directional link between loneliness and subjective well-being. Changes in neural function can help explain this association. Loneliness and isolation, for example, have been linked to dysfunction in the ventral striatum and the limbic system, two brain regions that regulate motivation and stress responsiveness, respectively (Beller et al., 2018). Physiological symptoms such as increased plasma and urinary cortisol levels and increased stress reactivity accompany these neural changes (Vitale et al., 2022). Prolonged social isolation has been linked to significant changes in brain morphology. When compared to controls, there were significant reductions in brain-derived neurotrophic factor concentrations and gray matter volume in the dorsolateral and orbitofrontal cortex, as well as the hippocampus (Gonder et al., 2022).
Notably, research on chronic loneliness and the amygdala yielded conflicting results. Some researchers emphasized the importance of an intact amygdala for maintaining social relationships (Scheele et al., 2019), while others claimed that an intact amygdala is not required to maintain social relationships (Becker et al., 2012). In the face of this debate, researchers have begun using large-scale brain morphology studies to investigate the sex-dependent effects of loneliness on brain volume, particularly in the amygdala and the ventromedial prefrontal cortex (vmPFC) (Mikics et al., 2018). Smaller amygdala volumes were found in lonely men but not in lonely women, and this pattern was reversed for the vmPFC volume (smaller in lonely women but not lonely men). Researchers also suggest that prospective longitudinal studies are needed to track sex-specific morphological changes associated with chronic loneliness. Furthermore, the default mode network (DMN), which has been identified as a key component of perceived social isolation (Lieberz et al., 2021), showed volume deviations and functional communication changes that were more prominent in lonely men than in lonely women.
Mechanism research can benefit from animal models. For example, animal studies on the effects of social isolation have observed similar physiological symptoms such as increased corticosterone (the rodent equivalent of human cortisol) as well as altered motivation, increased stress responsiveness, and dysregulation of the mesocortical dopamine and limbic systems (Vitale et al., 2022). Animal studies also show an association between social isolation and hippocampal neurogenesis (Mikics et al., 2018). From an evolutionary standpoint, loneliness in humans serves as an adaptive function and evolutionary coping strategy to promote behavioral changes (Spithoven et al., 2019). For example, studies suggest that loneliness triggers the need for social connection, which is analogous to the need for food in starvation (Tomova et al., 2022).
The development of neurobiologically informed interventions for loneliness is critically dependent on a better understanding of structural and functional neural changes in the brain associated with chronic feelings of social isolation. Given that the extended lockdown during COVID-19 may promote a transition from acute to chronic loneliness, more research is needed to investigate possible causal pathways that lead to social withdrawal and chronic loneliness.
A range of strategies can be employed to mitigate loneliness, including treatment for mental health problems that are risk factors for loneliness, prevention of the transition from acute to chronic loneliness, and increased social support or social contact. According to a recent meta-analysis, a variety of psychological interventions (e.g., cognitive-behavioral therapy, gratitude, reminiscence, mindfulness, integrative, social skills and social identity approaches) are effective in reducing feelings of loneliness (Hickin et al., 2021). In addition, preventative research has concentrated on developing and evaluating internet- or tele-delivered approaches that may enable more scalable and accessible interventions for chronic loneliness (Bruce et al., 2021). Furthermore, another meta-analysis found that interventions that simply attempted to increase social support or social contact were less effective than those that attempted to target the maladaptive cognitions that foster loneliness (Masi et al., 2011), implying that individuals may need to play a more active role in breaking the cycle of loneliness (compared to replying on social support). So far, no studies have looked at brain activity or connectivity in lonely people who have had successful interventions. Future prospective studies are needed to distinguish predisposing brain alterations that make people vulnerable to chronic loneliness from alterations caused by prolonged loneliness.
The time is right for loneliness research to take on these challenges – one meta-analysis covering over 215000 participants discovered a small but significant increase in loneliness during the COVID-19 pandemic (Ernst et al., 2022). Recently, researchers have proposed more monitoring of feelings of social connectedness as well as research into risk and protective factors. Furthermore, the study found that, in addition to social isolation, social loss is a growing trigger of loneliness This shared global experience has highlighted the importance of continuing research into the neural underpinnings of not only loneliness, but also loss and grief processing.
Humans are social creatures, so maintaining healthy and positive social interaction is an essential component of human existence. Investigating loneliness through various lenses may lead to a novel approach to improving the quality of life for those suffering from these conditions.
References
Alsulami, G., Rice, A. M., & Kidd, L. (2019). Prospective repeated assessment of self-reported sleep quality and sleep disruptive factors in the intensive care unit: Acceptability of daily assessment of sleep quality. BMJ Open, 9(6). ProQuest One Academic; Psychology Database. https://doi.org/10.1136/bmjopen-2019-029957
Aust, S., Härtwig, E. A., Koelsch, S., Heekeren, H. R., Heuser, I., & Bajbouj, M. (2014). How emotional abilities modulate the influence of early life stress on hippocampal functioning. Social Cognitive and Affective Neuroscience, 9(7), 1038–1045. APA PsycInfo®. https://doi.org/10.1093/scan/nst078
Becker, B., Mihov, Y., Scheele, D., Kendrick, K. M., Feinstein, J. S., Matusch, A., Aydin, M., Reich, H., Urbach, H., Oros-Peusquens, A.-M., Shah, N. J., Kunz, W. S., Schlaepfer, T. E., Zilles, K., Maier, W., & Hurlemann, R. (2012). Fear processing and social networking in the absence of a functional amygdala. Biological Psychiatry, 72(1), 70–77. APA PsycInfo®. https://doi.org/10.1016/j.biopsych.2011.11.024
Beller, J., & Wagner, A. (2018). Loneliness, social isolation, their synergistic interaction, and mortality. Health Psychology, 37(9), 808-813. https://doi.org/10.1037/hea0000605
Boyle, A. R., & Davis, H. (2006). Early screening and assessment of alcohol and substance abuse in the elderly: Clinical implications. Journal of Addictions Nursing, 17(2), 95–103. APA PsycInfo®. https://doi.org/10.1080/10884600600668229
Bruce, M. L., Pepin, R., Marti, C. N., Stevens, C. J., & Choi, N. G. (2021). One year impact on social connectedness for homebound older adults: Randomized controlled trial of tele-delivered behavioral activation versus tele-delivered friendly visits. The American Journal of Geriatric Psychiatry, https://doi.org/10.1016/j.jagp.2021.05.005
Buecker, S., & Horstmann, K. T. (2021). Loneliness and social isolation during the COVID-19 pandemic: A systematic review enriched with empirical evidence from a large-scale diary study. European Psychologist, 26(4), 272-284. https://doi.org/10.1027/1016-9040/a000453
Burke, T. J., & Segrin, C. (2014). Bonded or stuck? Effects of personal and constraint commitment on loneliness and stress. Personality and Individual Differences, 64, 101–106. APA PsycInfo®. https://doi.org/10.1016/j.paid.2014.02.027
Burns, A., Leavey, G., Ward, M., & O’Sullivan Roger. (2022). The impact of loneliness on healthcare use in older people: Evidence from a nationally representative cohort. Journal of Public Health, 30(3), 675–684. Agricultural & Environmental Science Collection; ProQuest One Academic. https://doi.org/10.1007/s10389-020-01338-4
Cacioppo, J. T., & Cacioppo, S. (2018). The growing problem of loneliness. The Lancet, 391(10119), 426. APA PsycInfo®. https://doi.org/10.1016/S0140-6736(18)30142-9
Cacioppo, J. T., & Patrick, W. (2008). Review of Human: The science behind what makes us unique. Nature Neuroscience, 11(10), 1119. APA PsycInfo®. https://doi.org/10.1038/nn1008-1119
Cacioppo, J. T., PhD, Burleson, M. H., PhD, Poehlmann, K. M., PhD, Malarkey, W. B., MD, Kiecolt-glaser, J. K., PhD, Berntson, G. G., PhD, Uchino, B. N., PhD, & Glaser, R., PhD. (2000). Autonomic and neuroendocrine responses to mild psychological stressors: Effects of chronic stress on older women. Annals of Behavioral Medicine, 22(2), 140–148. ProQuest One Academic; Psychology Database. https://doi.org/10.1007/BF02895778
Cavicchioli, M., & Maffei, C. (2020). Rejection sensitivity in borderline personality disorder and the cognitive–affective personality system: A meta-analytic review. Personality Disorders: Theory, Research, and Treatment, 11(1), 1–12. APA PsycArticles®. https://doi.org/10.1037/per0000359
Chang, E. C., Muyan, M., & Hirsch, J. K. (2015). Loneliness, positive life events, and psychological maladjustment: When good things happen, even lonely people feel better! Personality and Individual Differences, 86, 150–155. APA PsycInfo®. https://doi.org/10.1016/j.paid.2015.06.016
Clark, D. M. T., Loxton, N. J., & Tobin, S. J. (2015). Multiple mediators of reward and punishment sensitivity on loneliness. Personality and Individual Differences, 72, 101–106. APA PsycInfo®. https://doi.org/10.1016/j.paid.2014.08.016
Clark, M. S., Bond, M. J., & Hecker, J. R. (2007). Environmental stress, psychological stress and allostatic load. Psychology, Health & Medicine, 12(1), 18–30. APA PsycInfo®. https://doi.org/10.1080/13548500500429338
Cudjoe, T. K. M., & Kotwal, A. A. (2020). “Social distancing” amid a crisis in social isolation and loneliness. Journal of the American Geriatrics Society, 68(6), E27–E29. APA PsycInfo®. https://doi.org/10.1111/jgs.16527
Elmelid, A., Stickley, A., Lindblad, F., Schwab-Stone, M., Henrich, C. C., & Ruchkin, V. (2015). Depressive symptoms, anxiety and academic motivation in youth: Do schools and families make a difference? Journal of Adolescence, 45, 174–182. APA PsycInfo®. https://doi.org/10.1016/j.adolescence.2015.08.003
Ernst, M., Niederer, D., Werner, A. M., Czaja, S. J., Mikton, C., Ong, A. D., Rosen, T., Brähler, E., & Beutel, M. E. (2022). Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. American Psychologist, https://doi.org/10.1037/amp0001005
Freak-Poli, R., Ryan, J., Tran, T., Owen, A., McHugh Power, J., Berk, M., Stocks, N., Gonzalez-Chica, D., Lowthian, J. A., Fisher, J., & Byles, J. (2021). Social isolation, social support and loneliness as independent concepts, and their relationship with health-related quality of life among older women. Aging & Mental Health. APA PsycInfo®. https://doi.org/10.1080/13607863.2021.1940097
Gerst-Emerson, K., & Jayawardhana, J. (2015). Loneliness as a Public Health Issue: The Impact of Loneliness on Health Care Utilization Among Older Adults. American Journal of Public Health, 105(5), 1013–1019. Agricultural & Environmental Science Collection; ProQuest One Academic; Psychology Database.
Gonder, M. E., Orr, W. N., & Khan, T. W. (2022). The Impact of Isolation During COVID-19 on Chronic Musculoskeletal Pain in the Geriatric Population: A Narrative Review. Pain Physician, 25(2), E185–E191. Coronavirus Research Database; ProQuest One Academic.
Gottlieb, B. H., & Bergen, A. E. (2010). Social support concepts and measures. Journal of Psychosomatic Research, 69(5), 511–520. APA PsycInfo®. https://doi.org/10.1016/j.jpsychores.2009.10.001
Hänsel, A., Hong, S., Cámara, R. J. A., & von Känel, R. (2010). Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neuroscience and Biobehavioral Reviews, 35(1), 115–121. APA PsycInfo®. https://doi.org/10.1016/j.neubiorev.2009.12.012
Hawkley, L. C., Masi, C. M., Berry, J. D., & Cacioppo, J. T. (2006). Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging, 21(1), 152–164. APA PsycArticles®. https://doi.org/10.1037/0882-7974.21.1.152
Hawkley, L. C., Thisted, R. A., Masi, C. M., & Cacioppo, J. T. (2010). Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychology and Aging, 25(1), 132–141. APA PsycArticles®. https://doi.org/10.1037/a0017805
Hickin, N., Käll, A., Shafran, R., Sutcliffe, S., Manzotti, G., & Langan, D. (2021). The effectiveness of psychological interventions for loneliness: A systematic review and meta-analysis. Clinical Psychology Review, 88, 14. APA PsycInfo®. https://doi.org/10.1016/j.cpr.2021.102066
Hwang, T.-J., Rabheru, K., Peisah, C., Reichman, W., & Ikeda, M. (2020). Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics, 32(10), 1217–1220. APA PsycInfo®. https://doi.org/10.1017/S1041610220000988
Käll, A., Shafran, R., Lindegaard, T., Bennett, S., Cooper, Z., Coughtrey, A., & Andersson, G. (2020). A common elements approach to the development of a modular cognitive behavioral theory for chronic loneliness. Journal of Consulting and Clinical Psychology, 88(3), 269–282. APA PsycInfo®. https://doi.org/10.1037/ccp0000454
Kennedy, S., Kiecolt-Glaser, J. K., & Glaser, R. (1988). Immunological consequences of acute and chronic stressors: Mediating role of interpersonal relationships. British Journal of Medical Psychology, 61(1), 77–85. APA PsycInfo®. https://doi.org/10.1111/j.2044-8341.1988.tb02766.x
Kiesow Hannah, Uddin, L. Q., Bernhardt, B. C., Kable, J., & Bzdok Danilo. (2021). Dissecting the midlife crisis: Disentangling social, personality and demographic determinants in social brain anatomy. Communications Biology, 4(1). ProQuest One Academic. https://doi.org/10.1038/s42003-021-02206-x
Killgore, W. D. S., Cloonan, S. A., Taylor, E. C., Lucas, D. A., & Dailey, N. S. (2020). Loneliness during the first half-year of COVID-19 lockdowns. Psychiatry Research, 294, 2. APA PsycInfo®. https://doi.org/10.1016/j.psychres.2020.113551
Lee, S. L. J., Horsfield, J. A., Black, M. A., Rutherford, K., & Gemmell, N. J. (2018). Identification of sex differences in zebrafish (Danio rerio) brains during early sexual differentiation and masculinization using 17α-methyltestoterone. Biology of Reproduction, 99(2), 446–460. ProQuest One Academic. https://doi.org/10.1093/biolre/iox175
Leichsenring, F. (2004). Quality of depressive experiences in borderline personality disorders: Differences between patients with borderline personality disorder and patients with higher levels of personality organization. Bulletin of the Menninger Clinic, 68(1), 9–22. ProQuest One Academic; Psychology Database.
Lieberz, J., Simone G. Shamay‐Tsoory, Saporta, N., Esser, T., Kuskova, E., Birgit Stoffel‐Wagner, Hurlemann, R., & Scheele, D. (2021). Loneliness and the Social Brain: How Perceived Social Isolation Impairs Human Interactions. Advanced Science, 8(21). ProQuest One Academic. https://doi.org/10.1002/advs.202102076
Masi, C. M., Chen, H.-Y., Hawkley, L. C., & Cacioppo, J. T. (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. APA PsycInfo®. https://doi.org/10.1177/1088868310377394
Meisters, R., Putrik, P., Westra, D., Bosma, H., Ruwaard, D., & Jansen, M. (2021). Is Loneliness an Undervalued Pathway between Socio-Economic Disadvantage and Health? International Journal of Environmental Research and Public Health, 18(19), 10177. Agricultural & Environmental Science Collection; Coronavirus Research Database; ProQuest One Academic. https://doi.org/10.3390/ijerph181910177
Mikics, É., Guirado, R., Umemori, J., Tóth, M., Biró, L., Miskolczi, C., Balázsfi, D., Zelena, D., Castrén, E., Haller, J., & Karpova, N. N. (2018). Social Learning Requires Plasticity Enhanced by Fluoxetine Through Prefrontal Bdnf-TrkB Signaling to Limit Aggression Induced by Post-Weaning Social Isolation. Neuropsychopharmacology, 43(2), 235–245. ProQuest One Academic; Psychology Database. https://doi.org/10.1038/npp.2017.142
Morneau‐Vaillancourt, G., Andlauer, T. F. M., Ouellet‐Morin, I., Paquin, S., Brendgen, M. R., Vitaro, F., Gouin, J., Séguin, J. R., Gagnon, É., Cheesman, R., Forget‐Dubois, N., Rouleau, G. A., Turecki, G., Tremblay, R. E., Côté, S. M., Dionne, G., & Boivin, M. (2021). Polygenic scores differentially predict developmental trajectories of subtypes of social withdrawal in childhood. Journal of Child Psychology and Psychiatry, 62(11), 1320–1329. APA PsycInfo®. https://doi.org/10.1111/jcpp.13459
Otten, D., Ernst, M., Tibubos, A. N., Brähler, E., Fleischer, T., Schomerus, G., Wild, P. S., Zöller, D., Binder, H., Kruse, J., Johar, H., Atasoy, S., Grabe, H. J., Ladwig, K.-H., Münzel, T., Völzke, H., König, J., & Beutel, M. E. (2022). Does social support prevent suicidal ideation in women and men? Gender-sensitive analyses of an important protective factor within prospective community cohorts. Journal of Affective Disorders, 306, 157–166. APA PsycInfo®. https://doi.org/10.1016/j.jad.2022.03.031
Pan, L., Xu, Q., Kuang, X., Zhang, X., Fang, F., Gui, L., Li, M., Tefsen, B., Zha, L., & Liu, H. (2021). Prevalence and factors associated with post-traumatic stress disorder in healthcare workers exposed to COVID-19 in Wuhan, China: A cross-sectional survey. BMC Psychiatry, 21, 9. APA PsycInfo®. https://doi.org/10.1186/s12888-021-03589-1
Perron, J. L., Cleverley, K., & Kidd, S. A. (2014). Resilience, loneliness, and psychological distress among homeless youth. Archives of Psychiatric Nursing, 28(4), 226–229. APA PsycInfo®. https://doi.org/10.1016/j.apnu.2014.05.004
Pietrzak, R. H., Javier, F. G., Krystal, J. H., & Southwick, S. M. (2021). Subthreshold post-traumatic stress disorder as a risk factor for post-traumatic stress disorder: Results from a sample of USA veterans. The British Journal of Psychiatry, 219(2), 456–459. ProQuest One Academic; Psychology Database. https://doi.org/10.1192/bjp.2021.17
Scheele, D., Zimbal, S., Feinstein, J. S., Delis, A., Neumann, C., Mielacher, C., Philipsen, A., & Hurlemann, R. (2019). Treatment-resistant depression and ketamine response in a patient with bilateral amygdala damage. The American Journal of Psychiatry, 176(12), 982–986. APA PsycInfo®. https://doi.org/10.1176/appi.ajp.2019.18101219
Science; New Findings from University of Oxford in the Area of Science Reported (10,000 social brains: Sex differentiation in human brain anatomy). (2020, April 10). Health & Medicine Week, 3241. ProQuest One Academic.
Segerstrom, S. C., & Miller, G. E. (2004). Psychological Stress and the Human Immune System: A Meta-Analytic Study of 30 Years of Inquiry. Psychological Bulletin, 130(4), 601–630. APA PsycArticles®. https://doi.org/10.1037/0033-2909.130.4.601
Sermat, V. (1984). Review of Loneliness: A Sourcebook of Current Theory, Research and Therapy. Canadian Psychology/Psychologie Canadienne, 25(4), 301–303. APA PsycInfo®. https://doi.org/10.1037/h0080959
Sermat, V. (1984). Review of 0RW1S34RfeSDcfkexd09rT2Loneliness: A Sourcebook of Current Theory, Research and Therapy1RW1S34RfeSDcfkexd09rT2. Canadian Psychology/Psychologie Canadienne, 25(4), 301-303. https://doi.org/10.1037/h0080959
Spithoven, A. W. M., Cacioppo, S., Goossens, L., & Cacioppo, J. T. (2019). Genetic contributions to loneliness and their relevance to the evolutionary theory of loneliness. Perspectives on Psychological Science, 14(3), 376–396. APA PsycInfo®. https://doi.org/10.1177/1745691618812684
Teicher, M. H., Samson, J. A., Anderson, C. M., & Ohashi, K. (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience, 17(10), 652–666. APA PsycInfo®. https://doi.org/10.1038/nrn.2016.111
Tomova, L., Wang, K. L., Thompson, T., Matthews, G. A., Takahashi, A., Tye, K. M., & Saxe, R. (2022). “Acute social isolation evokes midbrain craving responses similar to hunger”: Correction. Nature Neuroscience, 25(3), 399. APA PsycInfo®. https://doi.org/10.1038/s41593-021-01004-2
Vitale, E. M., & Smith, A. S. (2022). Neurobiology of Loneliness, Isolation, and Loss: Integrating Human and Animal Perspectives. Frontiers in Behavioral Neuroscience, https://doi.org/10.3389/fnbeh.2022.846315
Wolf, L. D., & Davis, M. C. (2014). Loneliness, daily pain, and perceptions of interpersonal events in adults with fibromyalgia. Health Psychology, 33(9), 929–937. APA PsycArticles®. https://doi.org/10.1037/hea0000059
Wols, A., Scholte, R. H. J., & Qualter, P. (2015). Prospective associations between loneliness and emotional intelligence. Journal of Adolescence, 39, 40–48. APA PsycInfo®. https://doi.org/10.1016/j.adolescence.2014.12.007
Zhang, N., Abler, L., Yu, B., & Pan, S. (2014). Understanding the Meaning of Short-Term, Yiyeqing Relationships and How They are Formed: Implications for Condom Use in Liuzhou, China. AIDS and Behavior, 18(2), 126–134. Agricultural & Environmental Science Collection; ProQuest One Academic; Psychology Database. https://doi.org/10.1007/s10461-013-0489-x
Related Posts
How Genetic Engineering Can Responsibly Revolutionize Healthcare Treatment
Source: iStock At just 3 months old, Victoria Gray was...
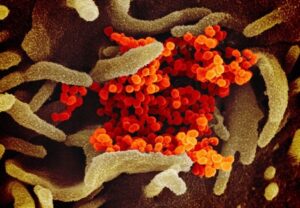
Read MoreThe COVID Brain
Cover Image: The Structure of the Coronavirus. (Source: Wikimedia Commons,...
Read MoreRisk of Death Among Recently Released Inmates
Figure 1: While healthcare inequity is certainly an issue while...
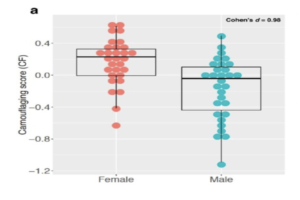
Read MoreAutism Spectrum Disorder and Gender: The Case for Expanding the Autistic Phenotype
This article was originally submitted to the Modern MD competition...
Read MoreThe Positives of Plushies: Stuffed Animals Have Benefits for Children and Adults
Figure: A young girl sleeps with a teddy bear in...
Read MoreThe “Old Friends” Hypothesis and the COVID-19 Pandemic
Authors: Sakeena Badrane1, Vivek Babu2, Sanah Handu1 1University of Pittsburgh,...
Read MoreMingcong Tang