This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023 Summer Program.

Source: Unsplash, Ashkan Forouzani
As of 2023, almost 1.9 billion people around the world live in impoverished conditions –24% of the global population1. In the US, poverty is especially concentrated in more rural areas. Based on census data from November 2022, the poverty rate in non-metro areas appears to be 15.4% while the poverty rate in metro areas is 11.9%. Poverty in these non-metro areas is persistent and remains at high rates2.
A main concern for rural areas is acquiring and maintaining healthcare professionals. Various factors can negatively influence a medical professional’s decision to stay in rural towns. Healthcare professionals desire advanced medical equipment and qualified staff, both of which are more difficult to find in rural areas3. With insufficient budgets, buying and installing expensive equipment in rural areas is close to impossible; an inability to accommodate health professionals’ preferences, poses an obstacle and leaves these towns with inadequate human resources. Medical professionals also tend to consider the skills and knowledge of the community they choose to settle in3. They prefer areas with good schooling systems and medical communities, primarily to be able to pursue their own interests and goals. Without proper facilities and partners, medical professionals are restricted to their specific job role as opposed to being able to grow and learn in a medical community.
Healthcare is not just limited by geographic location. Unfortunately, race is still a factor that effects healthcare access and treatment. During the COVID-19 pandemic, African Americans comprised about 43% of the deaths in Illinois although they only make up 15% of the population4. Illinois was not the only state with this sort of pattern – other states and cities exhibit similar disparities. The high death rates of African Americans during the pandemic are a direct consequence of generations worth of systematic racism, contributing to the present situation where many African Americans are still living in poverty. Still more than twice as many African Americans live below the poverty line than White and Asian Americans, even though the poverty rate for African Americans has been declining5. This makes it relatively more difficult to afford health care and obtain proper treatment. Furthermore, the greater likelihood of living in a household with more limited space increased the risk of exposure to COVID-19. It is not just African Americans, but Hispanic communities as well that are facing higher poverty rates6.
To reduce the gap of healthcare access, various community efforts are being taken. Numerous organizations are working towards helping those in need, such as Doctors without Borders, UNICEF, and Health Poverty Action. But there is clearly still much more work to be done. As a community, we can encourage the distribution of medical insurance with the aim to provide sufficient care to every person.
References
- Peer, A. (2023). Global poverty: Facts, FAQs, and how to help. World Vision. https://www.worldvision.org/sponsorship-news-stories/global-poverty-facts
- Rural Poverty & Well-Being. USDA Economic Research Service. https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/
- Pender et al. (2023). Linkages Between Rural Community Capitals and Healthcare Provision: A Survey of Small Rural Towns in Three U.S. Regions. USDA Economic Research Service. https://www.ers.usda.gov/publications/pub-details/?pubid=106138
- Smedley, Brian. Why Is Covid-19 Disproportionately Affecting Black and Latino Americans? American Psychological Association. https://www.apa.org/news/podcasts/speaking-of-psychology/african-americans-latinos-covid-19
- Creamer, John. (2020). Inequalities Persist Despite Decline in Poverty for All Major Race and Hispanic Origin Groups. United States Census Bureau. https://www.census.gov/library/stories/2020/09/poverty-rates-for-blacks-and-hispanics-reached-historic-lows-in-2019.html
- Cené et al. (2023). Racial Health Equity and Social Needs Interventions: A Review of a Scoping Review. Journal of the American Medical Association 6 (1): e2250654
Related Posts
How Genetic Engineering Can Responsibly Revolutionize Healthcare Treatment
Source: iStock At just 3 months old, Victoria Gray was...
Read MoreThe Public Health Crisis of Alzheimer’s Disease in African American and Hispanic Populations
This publication is in proud partnership with Project UNITY’s Catalyst...
Read MoreA Novel Mental Health Literacy Education Program for Pre-Teens
Figure: A typical elementary school classroom in Japan (Cassidy, 2005). Source:...
Read MoreThe Role of Biometrics in Healthcare
This publication is in proud partnership with Project UNITY’s Catalyst...
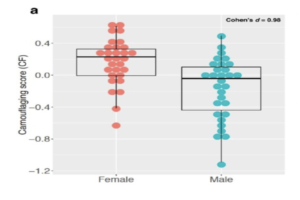
Read MoreAutism Spectrum Disorder and Gender: The Case for Expanding the Autistic Phenotype
This article was originally submitted to the Modern MD competition...
Read MoreThe Public Health Humanitarian Crisis in Ukraine
This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023...
Read MoreShaila Pochiraju