Source: 허동은교수, Wikimedia Commons, CC BY-SA 4.0
Introduction
Recent years have seen notable advancements in the field of regenerative medicine, with an emphasis on the creation of artificial organs and organ-on-a-chip technologies. These innovative developments have the potential to transform healthcare by tackling pressing medical issues including the lack of organ donors for transplantation and the demand for more precise and effective drug discovery techniques. To better understand how artificial organs and organs-on-a-chip are changing healthcare and enhancing patient outcomes, this article will examine the current state of these technologies.
The lack of organ donors for transplantation is a critical issue on a global scale. Despite improvements in immunosuppressive medicines and transplantation methods, there is still a huge demand for organs. Artificial organs are designed to mimic the shape and functionality of their natural counterparts, providing hope for transplant recipients – thus, they may be used to overcome constraints like the lack of enough organ donors to meet demand and address issues such as organ rejection, immunosuppressive drug dependence, and the scarcity of compatible donors. These modified organs can be tailor-made for each individual patient by obtaining the patient’s cells and inducing them to differentiate into the specific cell types found in the desired organ. As a result, these modified organs lower the chance of rejection and eliminate the need for ongoing immunosuppressive medicine. Furthermore, since they can be produced on demand, artificial organs have the potential to transcend geographical boundaries, decreasing the need for organ transportation and increasing access to life-saving therapies.
How are artificial organs and organs-on-a-chip improving healthcare and enhancing patient outcomes? By exploring the results of studies that cite these new technologies, we can understand their present state, difficulties, and potential to transform healthcare and enhance patients’ lives all around the world.
Experiments and Findings
Artificial Organs
The creation of functioning substitutes for organs like the heart, kidney, liver, and pancreas has advanced significantly in recent years. For instance, biomaterials and patient-derived cells have been combined to build bioengineered hearts1. These mechanical hearts may be able to offer patients with heart failure long-term remedies. Similar research has been done on prosthetic kidneys. For patients with end-stage renal illness, these designed kidneys strive to mimic the filtration and reabsorption capacities of the natural organ. To construct artificial kidneys with improved functionality, researchers have created novel techniques like bioprinting and microfluidic systems2. These developments have a lot of potential for satisfying the expanding demand for kidney transplants and improving the quality of life for patients with renal failure.
Organs-on-a-Chip
The ability of organs-on-a-chip to replicate the composition and operation of human organs has attracted a lot of interest. What are organs on a chip exactly – and how do they differ from artificial organs? According to Takebe et al. (2017), organs on a chip are microfabricated devices consisting of chambers lined with living human cells that precisely imitate the physiology of particular organs. Currently, they have been used in cancer research as platforms to examine how tumors grow, invade surrounding tissue, and react to therapeutic interventions. Compared to conventional cell cultures or animal models, these tools offer a more accurate portrayal of the tumor microenvironment, allowing researchers to learn more about cancer biology and test prospective treatment candidates in settings that are more relevant to their research3.
Beyond cancer, researchers are using these tools to study Alzheimer’s disease, diabetes, and other conditions, offering insightful information about the course of the disease and prospective treatment targets. As an illustration, liver-on-a-chip devices have been created to mimic the complex metabolic processes of the liver, enabling researchers to examine drug metabolism, toxicity, and the course of illness. Research on neurodegenerative illnesses like Parkinson’s and Alzheimer’s has also benefited from using organ-on-a-chip technology. Researchers may study disease causes, test new treatments, and check for neurotoxicity using these devices since they can mimic the complex cellular interactions and neuronal activity seen in the human brain4.
Impact
Artificial organs and organs-on-a-chip have a significant impact, but the path to clinical trials for these tools involves several stages of research and development, with the ultimate goal of achieving safe and effective implementation in human patients. Currently, researchers are in the preclinical phase, where artificial organs are being extensively tested in laboratory settings and animal models to evaluate their functionality, safety, and efficacy. This preliminary work will help to refine their design and optimize performance before advancing to human trials.
Recently, specific pharmaceutical companies have recognized the potential of organ-on-a-chip platforms that offer more physiologically relevant models for studying drug effects. The use of these platforms can help speed up the process of developing new drugs, making them safer and more efficient. By leveraging this technology, companies can conduct a thorough screening of drug candidates to potentially reduce the cost and time associated with traditional drug discovery approaches. The integration of organs-on-a-chip into pharmaceutical research and development represents a promising advancement in the field, paving the way for more efficient and personalized therapy.
Conclusion
Together, artificial organs and organs-on-a-chip development offer a potential answer to the organ shortage and serve as more effective platforms for drug discovery. Several obstacles still exist, however, to their implementation. One of the main issues that must be resolved for clinical translation to be effective is biocompatibility, which is the ability of a material or device to maintain structural integrity and perform its intended function within a biological system without causing undesirable effects like inflammation or toxicity. Other important issues include the long-term durability of the organs in the body and the scalability of their production (i.e., whether these artificial organs be produced efficiently for many patients at a time). Also, to ensure the effectiveness of these technologies, defined procedures and legal frameworks must be established. Even while issues with biocompatibility, long-term functionality, and regulatory frameworks still exist, the current research and interdisciplinary cooperation show a lot of promise. The continuous research and application of artificial organs and organs-on-a-chip will pave the way for better patient outcomes and individualized therapy, which is the future of healthcare.
References
- Dvir, T., et al. Nanowired three-dimensional cardiac patches. Nature Nanotechnology 6(11), 720-725 (2011).
- Humes, H. D., & MacKay, S. M. Clinical applications of renal cell therapy. Seminars in nephrology 39(1), 20-29 (2019).
- Takebe, T., et al. Engineering organs-on-chips. Cell Stem Cell 21(3), 297-311 (2017).
- Bhatia, S. N., & Ingber, D.E. Microfluidic organs-on-chips. Nature Biotechnology 32(8), 760-772 (2014).
Related Posts
Medical Overtreatment in the United States: Causes, Consequences, and Solutions
This article was originally submitted to the Modern MD competition...
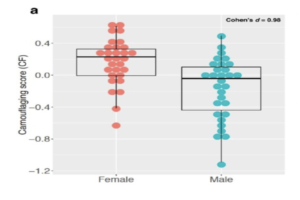
Read MoreAutism Spectrum Disorder and Gender: The Case for Expanding the Autistic Phenotype
This article was originally submitted to the Modern MD competition...
Read MoreBetter Zoning Through Inter-city Cooperation
Figure: High Density Housing (Source: Geograph Britain and Ireland, Author:...
Read MoreRisk of Death Among Recently Released Inmates
Figure 1: While healthcare inequity is certainly an issue while...
Read MorePreventing Peripheral Artery Disease in African Americans from Georgia: A Public Health Initiative
This publication is in proud partnership with Project UNITY’s Catalyst Academy 2024...
Read MoreA Field in Focus: Loneliness and Well-Being Research
Figure: An image of a woman wearing a mask, isolated...
Read MoreAnisha Shukla