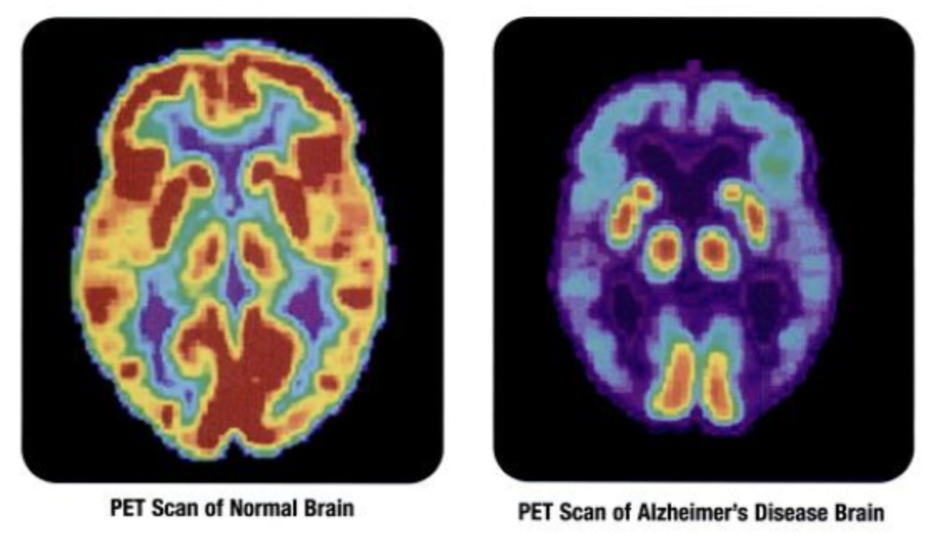
Cover Image: This image displays the differences between a normal brain and the brain of someone with Alzheimer’s disease on a PET scan. (Source: Wikimedia Commons, NIH)
Alzheimer’s Disease is one of the most prevalent degenerative neurological diseases within the human population. It is one of the most common causes of dementia and involves a consistent decline in social and behavioral skills over time, leading ultimately to individuals with Alzheimer’s depending entirely on others to function in daily life. This disease affects close to 6 million people in the United States who are 65 and older, and although medications are on the market that slow the progression of the illness (e.g., Aduhelm, Aricept, Exelon, and Razadyne), there is no treatment that can cure this disease (Mayo Clinic, 2021).
Of the existing treatments to slow Alzheimer’s progression, Aduhelm targets beta-amyloid, a protein fragment that forms plaques when accumulating and damages communication between nerve cells (Alzheimer’s Disease and Dementia, n.d.). Aricept, Exelon, and Razadyne work by a different mechanism. They prevent the breakdown of acetylcholine, which is a chemical that is integral to an individual’s memory and learning abilities. These medications enhance communication between neurons.
Scientists at City of Hope National Medical Center have created a miniature brain platform in order to better understand the pathological mechanism behind Alzheimer’s disease and to test other dementia drugs. They believe that a deeper understanding of the Alzheimer’s disease pathway on a biological level is essential to identifying its root causes and combatting them effectively.
The new platform developed by this team of researchers uses human induced pluripotent stem cells and brain organoids to find treatments for this disease. A brain organoid is an artificially grown organ that resembles the brain, and in this experiment, they represented a brain impacted by Alzheimer’s. They are used as an investigative model to understand how disease pathology operates. They exposed these models to mimic the age-associated blood-brain barrier breakdown since Alzheimer’s is an age-related illness. They then ran the organoids through different experiments in order to examine existing Alzheimer’s biomarkers, such as elevated levels of amyloid plaques and tau tangles. Amyloid plaques are misfolded proteins that emerge in the regions between neurons and can inhibit cognitive functions. Tau tangles are unusual accumulations of the protein Tau inside neurons. They work to disrupt brain cells that are essential to learning and memory (City of Hope, 2021).
With a working model of Alzheimer’s pathology in place, researchers can now test how different treatment molecules might alleviate Alzheimer’s symptoms (reduce biomarker levels) in the organoids. One area of focus is investigating the potential of combination therapies. Combination therapies have higher efficacies than single-target therapies because they involve multiple independent medications, potentially with different targets. Single-target therapies only target a specific protein or gene within the body. In the context of Alzheimer’s, it has previously been found that single-target therapies targeting either tau or amyloid did not substantially lower the levels of either protein (City of Hope, 2021). Combination therapy may be the solution to this dilemma.
In fact, just about any novel Alzhiemer’s drug, or combination of drugs, could be tested – and there are a number of them on the horizon. Some researchers are working on monoclonal antibodies to prevent plaques from forming and damaging brain cells. A monoclonal antibody is an engineered protein that works exactly like the antibodies of the immune system responding to various infections. By binding to a specific antigen (a molecule on a bacteria), a monoclonal antibody reinstates the correct immune response to combat these pathogens. Another drug known as saracatinib is being used to turn off a protein that allows synapses to start working again. In animal studies, treatment with the drug led to some reversal of memory loss (Mayo Clinic, 2021).
There are innumerable studies and cutting-edge clinical research being conducted by research centers and facilities all over the world. The treatment ideas and clinical research being tested primarily target the amyloid plaques and the tau proteins. While most of these testing methods are being performed on animals currently, scientists believe that, within the next few years, they could be piloted on human subjects. The use of human brain organoids is a very positive step in this direction.
References
City of Hope. (2021, August 2). Miniature brain models developed to study causes of Alzheimer’s disease and to test drugs in development: Most people suffering from the memory condition have late-onset Alzheimer’s disease, yet most studies have focused on early-onset inherited Alzheimer’s disease.. ScienceDaily. Retrieved September 13, 2021 from www.sciencedaily.com/releases/2021/08/210802160648.htm
Mayo Foundation for Medical Education and Research. (2021, June 26). Alzheimer’s disease. Mayo Clinic. Retrieved September 21, 2021, from https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/symptoms-causes/syc-20350447).
Mayo Foundation for Medical Education and Research. (2021, June 30). What new alzheimer’s treatments are on the horizon? Mayo Clinic. Retrieved September 21, 2021, from https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers-treatments/art-20047780.
Medications for memory, cognition and dementia-related behaviors. Alzheimer’s Disease and Dementia. (n.d.). Retrieved September 26, 2021, from https://www.alz.org/alzheimers-dementia/treatments/medications-for-memory.
Related Posts
Study Finds Anthrax Toxin as Possible Substitute for Painkillers
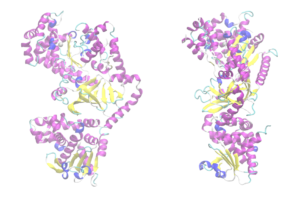
Figure: A computer representation of the anthrax toxin protein (Source:...
Read MoreHuman Endogenous Retroviruses Might Unlock a New Field of Neurodegenerative Disease Research
Figure 1: Researchers have found viral genetic materials within the...
Read MoreArtificial Intelligence for Mental Health Services
Source: Pavel Danilyuk In recent years, due to the pandemic...
Read MoreStaphylococcus epidermidis capable of 6-HAP production reduce host UV-induced tumors
Figure 1: The human microbiome is the collection of microorganisms...
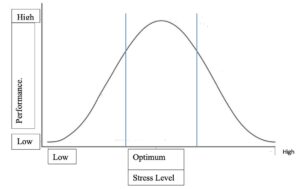
Read MoreRetitling Stress: A Look at the Yerkes-Dodson Law
Figure 1: This graph compares stress level with performance at...
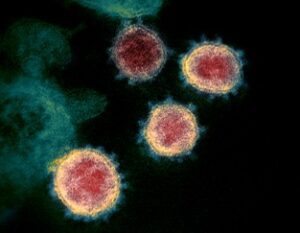
Read MoreCOVID-19 May Inflict Lasting Damage on the Central Nervous System
Figure 1: Transmission electron microscope image of the SARS-CoV-2 virus....
Read MoreKrithika Nathamuni