Figure: A computer representation of the anthrax toxin protein (Source: Wikimedia Commons, Ayacop)
For intensive surgery, opioids are often prescribed to help ease post-operative pain. They are very effective, but unfortunately also tend to be highly addictive, affecting about 15 million people every year, with an estimated cost of $35 billion in additional health care expenses (Pew Charitable Trusts, 2021). A new study published by scientists at Harvard Medical School outlines how a toxin from the bacterium Bacillus anthracis, a dangerous microbe that causes Anthrax, can actually be used as a pain treatment which lacks the addictive properties that typical opioids possess (Yang, 2021).
Previous studies have demonstrated the important role of dorsal root ganglion (DRG) neurons in the pain response – and scientists have even noted that prior injury induces molecular changes in these DRG neurons that make them hyper-susceptible to pain stimuli (Berta, 2017). These DRG neurons carry messages from the extremities to the brain and help produce the feeling of pain. In this new study, the authors concluded that the anthrax toxin is effective at targeting pain neurons (though the research is still highly experimental, and yet to be tested in humans). After showing that DRG neurons (in both mice and humans) possess the anthrax toxin receptor (ANTXR2) in abundance, the Harvard Medical School researchers subjected mice to treatment with anthrax toxin (partly modified so that it was less able to cause the negative symptoms of anthrax). In the mice, the toxin was able to bind to the ANTXR2 receptor in DRG neurons, and reduce pain behaviors.
A major implication of this study is that drastic improvements in the field of pain therapeutics are possible. The use of anthrax toxin itself as an analgesic (painkiller), or alternatively as a delivery tool to deliver other non-addictive painkillers into DRG neurons may be a much safer option. Since the toxin targets peripheral pain neurons specifically, not the brain like other common pain therapeutics, it is likely to have less addictive properties. The value of painkillers that don’t target the brain, which companies like Vertex Pharmaceuticals and Pfizer Inc. are also exploring, are dramatically positive – if an effective, but non-addictive painkiller becomes widely available, it would not only improve post-operative outcomes, but also help fight the raging opioid epidemic and potentially save hundreds of thousands of lives.
References
Berta, T., Qadri, Y., Tan, P. H., & Ji, R. R. (2017). Targeting dorsal root ganglia and primary sensory neurons for the treatment of chronic pain. Expert opinion on therapeutic targets, 21(7), 695–703. https://doi.org/10.1080/14728222.2017.1328057
“Can a Dangerous Microbe Offer a New Way to Silence Pain?” (2021). ScienceDaily, ScienceDaily, 20 Dec. 2021, https://www.sciencedaily.com/releases/2021/12/211220120629.htm.
“The High Price of the Opioid Crisis, 2021.” (2021). The Pew Charitable Trusts, https://www.pewtrusts.org/en/research-and-analysis/data-visualizations/2021/the-high-price-of-the-opioid-crisis-2021.
“Opioid Addiction: Medlineplus Genetics.” (2020). MedlinePlus, U.S. National Library of Medicine. https://medlineplus.gov/genetics/condition/opioid-addiction/#:~:text=Misuse%20of%20prescription%20opioids%20and,and%20addiction%20is%20rapidly%20increasing.
“Research and Pipeline.” (n.d.). Pipeline | Vertex Pharmaceuticals, https://www.vrtx.com/research-development/pipeline/.
Yang NJ, Isensee J, Neel DV, et al (2022). Anthrax toxins regulate pain signaling and can deliver molecular cargoes into ANTXR2+ DRG sensory neurons. Nat Neurosci. 25(2):168-179. doi:10.1038/s41593-021-00973-8
Related Posts
How the Human Microbiome Disables Drugs (And What We Can About It)
Scientists are studying the human microbiome and its ability to...
Read MoreInactivation of Type I Interferon Necessary for Myeloid-Derived Suppressor Cells
Figure 1: IFNγ (purple, bottom) is one kind of interferon,...
Read MoreCranial Cartography: A New Method for Visualizing Blood Vessels and Stem Cells in the Skull
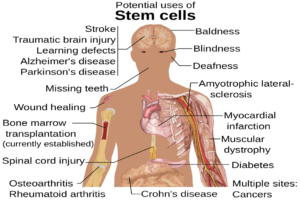
The diagram above displays the many potential uses of stem...
Read MoreInnovation Beyond All Barriers: The Arrival of a Life-Saving Treatment
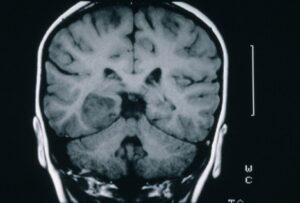
Figure 1:Magnetic resonance image (MRI) – coronal slice of a...
Read MoreThe Chernobyl Accident — A Natural Experiment for the Effects of Radiation on Humans
Figure 1: A monument (front left) to the meltdown at...
Read MoreJohn Parel