Figure: A neutrophil (yellow) ejecting a NET (green) to capture invading bacteria (purple) that are attacking a red blood cell (orange). (Source: Wikimedia Commons, CHDENK)
Neutrophils are a type of white blood cell involved in the innate immune response in most animals. These cells tend to be among the most numerous in the circulatory system; in fact, they are the single most abundant white blood cell in humans and make up to about 50% of the total blood cells in chimpanzees (Amulic et al., 2012; Stacey et al., 2021). Not only are they incredibly prevalent in the blood, neutrophils are generally among the “first-responders” to an immune reaction. Drawn to sites of inflammation by signals from the endothelial cells lining blood vessels, neutrophils undergo a process called “extravasation”, squeezing through the cracks between endothelial cells to enter damaged tissue. Once there, the neutrophils will respond to the situation based on what signals are being presented to it by the body’s cells as well as the source of inflammation, which can range from bodily damage to foreign pathogens. These responses include phagocytosing (engulfing and digesting) foreign threats and the body’s own damaged cells. Another response is the release of granules (self-contained organelles that contain various immunological effector molecules that either directly fight pathogens and/or recruit other immune cells to the scene) and/or reactive oxygen species (which are inflammatory and damaging to microbe and host alike). Additionally, the neutrophils can bind to microbes with effector surface proteins (often directly or indirectly destroying pathogens). Finally, they can undergo apoptosis (deliberate death of the cell) to release Neutrophil Extracellular Traps (NETs) (Amulic et al., 2012).
This last function, the intentional self-destruction of a cell to release a web-like trap is a process known as NETosis. NETs consist of DNA-binding proteins called histones, nuclear and mitochondrial DNA, and proteins with antimicrobial effects (see Figure 1 above). The DNA components provide the scaffolding and rope-like constitution of the NET. They were only recently discovered in 2004. First thought to mainly target bacteria and their virulence factors, which are effector molecules that are responsible for infection and/or damage to the host (Brinkmann et al., 2004), it is now known that NETs effectively target and neutralize bacteria, fungi, viruses, and possibly even multicellular parasites, (Papayannopoulos, 2018). It has been shown that the protein composition of the NET varies by the stimulus that induced the cell to destroy itself, but all NETs contain high amounts of antimicrobial proteins, especially the protease neutrophil elastase (Amulic et al., 2012; Brinkmann et al., 2004; Papayannopoulos, 2018).
It was recently discovered that upon binding to antigen-bound IgA class antibodies (proteins produced by B lymphocytes and plasma cells that are specific for a given antigen and predominantly found at mucous membranes), neutrophils undergo NETosis, releasing a slew of antiviral compounds that have been shown to trap and kill viruses. Thus, at the various mucous membranes (like those that line the mouth, nose, and urethra), if the immune system has fought off a given virus before and thus possesses memory B cells capable of producing antibodies against it, it will likely prevent reinfection by that virus via the NETs produced by this interaction. This may play a role in immunity conferred onto individuals by vaccines against different viruses, including polio and SARS-CoV-2, for example (Stacey et al., 2021).
NETs, like many immune functions, can have negative consequences for the host. Because NETs expose the immune system to the intracellular (inside) materials of the body’s cells, they run the risk of allowing for the development of an autoimmune response to various self-antigens. This autoimmunity may result in systemic lupus erythematosus (SLE), a disease marked by widespread inflammation and tissue damage along with red rashes on the skin, among other diseases (Amulic et al., 2012; Papayannopoulos, 2018). Furthermore, in releasing inflammatory molecules, NETs may result in further damage or a delay in repair to damage in various tissues (Papayannopoulos, 2018). In fact, this very possibility has been known to occur in severe cases of COVID-19, with there being significantly higher levels of NET components and neutrophils in the blood of patients who are required to be put on ventilators due to the infection and immune cell-mediated damage to the lungs (Zuo et al., 2020).
NETs can cause other problems as well. They may result in the blocking of various blood vessels by causing inflammation and trapping various cells and molecules, including the blood clot- forming platelets. The total effect is a large, sticky clot formed by NET and platelet-plug alike, resulting in various problems including the painful and dangerous Deep Vein Thrombosis (DVT), wherein a blot clot forms in a vein that is deep beneath the surface of the skin (Amulic et al., 2012; Papayannopoulos, 2018). In attempting to fight off some sort of infection, neutrophils and their NETs may end up doing more harm than good.
While much has been discovered about NETs recently, we still have much to learn about this undoubtedly vital function of neutrophils for immune defense. For example, it has been shown that neutrophils can release NETs without total destruction of themselves (although with the intentional release of some nuclear, but no mitochondrial, DNA) in response to Staphylococcus aureus bacteria – a common human pathogen that has a strong capacity to resist antibiotics (Pilsczek et al., 2010). This mechanism, whether it is unique to a response against S. aureus, and why it is not more widely used is certainly worth further research. Future studies will hopefully be able to reveal to us how to help optimize and regulate the NET response, providing maximal protection and minimal damage to our bodies when our neutrophils employ these molecular traps.
References
Amulic, B., Cazalet, C., Hayes, G. L., Metzler, K. D., & Zychlinsky, A. (2012). Neutrophil Function: From Mechanisms to Disease. Annual Review of Immunology, 30(1), 459–489. https://doi.org/10.1146/annurev-immunol-020711-074942
Brinkmann, V., Reichard, U., Goosmann, C., Fauler, B., Uhlemann, Y., Weiss, D. S., Weinrauch, Y., & Zychlinsky, A. (2004). Neutrophil Extracellular Traps Kill Bacteria. Science, 303(5663), 1532–1535. https://doi.org/10.1126/science.1092385
Papayannopoulos, V. (2018). Neutrophil extracellular traps in immunity and disease. Nature Reviews Immunology, 18(2), 134–147. https://doi.org/10.1038/nri.2017.105
Pilsczek, F. H., Salina, D., Poon, K. K. H., Fahey, C., Yipp, B. G., Sibley, C. D., Robbins, S. M., Green, F. H. Y., Surette, M. G., Sugai, M., Bowden, M. G., Hussain, M., Zhang, K., & Kubes, P. (2010). A novel mechanism of rapid nuclear neutrophil extracellular trap formation in response to Staphylococcus aureus. Journal of Immunology (Baltimore, Md.: 1950), 185(12), 7413–7425. https://doi.org/10.4049/jimmunol.1000675
Researchers discover unique “spider web” mechanism that traps, kills viruses. (2021, June 29). ScienceDaily. https://www.sciencedaily.com/releases/2021/06/210629101244.html
Stacey, H. D., Golubeva, D., Posca, A., Ang, J. C., Novakowski, K. E., Zahoor, M. A., Kaushic, C., Cairns, E., Bowdish, D. M. E., Mullarkey, C. E., & Miller, M. S. (2021). IgA potentiates NETosis in response to viral infection. Proceedings of the National Academy of Sciences, 118(27). https://doi.org/10.1073/pnas.2101497118
Zuo, Y., Yalavarthi, S., Shi, H., Gockman, K., Zuo, M., Madison, J. A., Blair, C., Weber, A., Barnes, B. J., Egeblad, M., Woods, R. J., Kanthi, Y., & Knight, J. S. (2020). Neutrophil extracellular traps in COVID-19. JCI Insight, 5(11). https://doi.org/10.1172/jci.insight.138999
Related Posts
The Neurobiological Basis of Autism
For more neuroscience news, check out the UnknownNow, a student...
Read MoreVideo Games Shape Childhood Cognitive Development
Source: Caleb Oquendo The first video game was introduced in...
Read MoreThe Connections Between Sleep and Memory
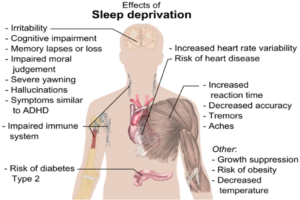
Figure: The image above displays the effects of sleep deprivation...
Read MoreCould This Be the First Drug to Slow the Progression of Alzheimer’s?
Figure 1: A cross section of a model brain Source: unsplash.com...
Read MoreWhy Future A.I Robots Should Be Created With Immutable Code Limiting Singularity
Figure: Sophia, the first robot citizen in the Global A.I...
Read MoreThe Effects of Friends and Family on Daily Stress
Figure 1: This figure shows several of the different effects...
Read MoreFrankie Carr