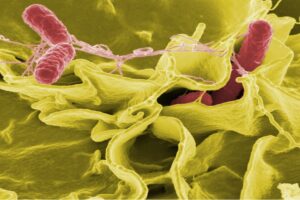
Extensive and irresponsible use of antimicrobial drugs is one of the leading causes of antimicrobial resistance. (Source: Wikimedia Commons, freestocks.org)
Most of us never thought that our lives would intersect with a pandemic. Yet, COVID-19 may not be the only pandemic witnessed in the 21st century. Antimicrobial resistance (AMR) is standing in the wings, ready to take centre-stage by 2050. Unlike other pandemics caused by new and unknown pathogens, AMR is driven by the evolution of microbes (bacteria, fungi, viruses, etc.) in the face of overexposure to antimicrobial drugs. As a result, increasingly robust versions of known pathogens replace their antimicrobial-susceptible predecessors. The WHO has included AMR under the top ten public health concerns (“Antimicrobial Resistance”, 2021). The statistics, though piecemeal, as countries haven’t started monitoring AMR closely, are alarming. According to a report by the BBC, antimicrobial resistance currently claims 700,000 lives per year and is predicted to cause the deaths of 10 million people a year by 2050, more than are currently taken by cancer (Walsh, 2014).
The incipient signs of this looming pandemic are already noticeable. For instance, the carbapenems, a class of broad-spectrum antibiotics used as last-resort treatment for severe bouts of pneumonia and urinary tract infections, are now ineffective in many patients globally. In 2019, the CDC documented the number of microbes that fell under the threat of AMR in the form of an AR Threats Report. The document included 21 types of bacteria and fungi, including those which pose an urgent threat in initiating a wave of AMR, as well as those microbes that were showing early signs of AMR (“2019 AR Threats Report”, 2019). Now that it is 2021, and the number of microbes resistant to available therapies is only snowballing with each passing year.
Antibacterial resistance, the most pervasive example of AMR, is a serious concern as it threatens to undo much of the progress made by modern medicine. Akin to a friends-turned-strangers situation, antibacterial resistance causes previously potent antibiotics to fail against the same bacteria against which they were once effective. The discovery of penicillin in the 1940s has long been heralded a major therapeutic win as it enabled seemingly incurable diseases like pneumonia and syphilis to be treated using non-toxic antibiotics. However, both pneumonia and syphilis have begun to show early signs of resistance and other bacterial infections like the STD gonorrhoea are turning impervious to existing treatments, leading to a rise in the number of hospitalisations and deaths due to microbial infections. According to the CDC, the United States witnesses about 2.8 million AMR infections, out which 35,000 people die as a result (“2019 AR Threats Report”, 2019). With an increasing number of antibiotics failing to serve their purpose, there is an urgent need to develop new antibiotics that can combat the rise of AMR.
It is interesting to note that to a certain degree, AMR is natural. Just as humans develop immunity against pathogens, it is expected that microbes would also develop “immunity” against the antimicrobials designed to kill them. However, what is concerning is the growing number of resistant strains. The overuse of antimicrobials such as antibiotics, their inappropriate prescription, and their extensive use in agriculture to fight crop-killing pests are the primary cause of resistance (Ventola, 2015). The concept of evolution holds true here— the more microbes exposed to antimicrobials, the better their chances of developing mechanisms to evade antimicrobial action and evolving into more hardy, drug-resistant species.
The implications of AMR are dire. AMR makes infectious diseases increasingly challenging to control, and the number of hospital stays for common illnesses is likely to increase manyfold. Routine operations may turn life-threatening as post-operation infections will not be as easily . The consequences of AMR extend even beyond epidemics of infectious disease, with indirect consequences for other diseases like cancer. Oncologists are worried that the widespread resistance against common antimicrobials could negatively impact cancer recovery. Pneumonia and sepsis are common post-treatment infections that plague cancer patients and are treated using antibiotics. In the event of AMR, patients could succumb to their post-treatment illnesses (Union for International Cancer Control, 2021).
AMR had already announcing its arrival, though to a lesser degree than the major medical catastrophe just described. As a result, we have time to prepare and protect ourselves from the effects of an AMR-driven pandemic. Several steps can be taken to ensure that the rise in AMR is kept under control. At the personal level, individuals should be sensible about taking antibiotics, actively discussing prescriptions with medical professionals and never taking them unnecessarily. At the medical level, over-prescription of antibiotics must be prevented at all costs. Policymakers and health professionals must continue to monitor signs of antimicrobial resistance so that we have a better idea of where we stand. This will help the scientific community and public policy officials make better-informed decisions and come up with strategic plans to combat the potential pandemic. Finally, it is critical for scientists and the pharmaceutical industry to invest in the research and development of new antibiotics, antimicrobials, and vaccines that can be used as alternatives when standard treatments fail on resistant microbial .
COVID-19 has shown us how pandemics can disrupt life as we know it. It would be foolish to ignore the signs that are glaring at us. While only time can tell us of the exact outcome of AMR, it is possible to harness the power of science and prudent policymaking to be better prepared when the next health crisis strikes the world.
References
2019 AR Threats Report. (2019). CDC. https://www.cdc.gov/drugresistance/biggest-threats.html
Antimicrobial Resistance. (2021).World Health Organisation. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
Antimicrobial Resistance and its impact on cancer care. (2021). Union for International Cancer Control. https://www.uicc.org/what-we-do/thematic-areas-work/antimicrobial-resistance-and-its-impact-cancer-care
Lee Ventola. (2015). The Antibiotic Resistance Crisis Part 1: Causes and Threats. Pharmacy & Therapeutics 40(4), 277-283. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/
Walsh, F. (2014). Superbugs to ‘kill more than cancer’ by 2050. BBC. https://www.bbc.co.uk/news/health-30416844
Related Posts
Targeting the Gut Microbiome to Keep Weight Off
Figure: Bacteria are essential for gut health because they help...
Read MoreA Field in Focus: Loneliness and Well-Being Research
Figure: An image of a woman wearing a mask, isolated...
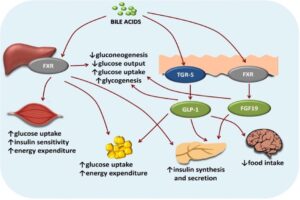
Read MoreBile Acid-Induced Satiety to Treat Obesity
Figure 1: Diagram of the effects of bile acids on...
Read MoreStaphylococcus epidermidis capable of 6-HAP production reduce host UV-induced tumors
Figure 1: The human microbiome is the collection of microorganisms...
Read MoreVirtual Healing: Trauma-Informed Solutions for Youth Addiction in Richmond, Virginia
This publication is produced in partnership with Project UNITY’s Catalyst...
Read MoreCOVID-19 Clinical Trials and Racial Disproportionality
Figure 1: A doctor drawing blood from a patient as...
Read MoreRamya Vishwanath