Figure 1: As Alzheimer’s disease research begins to shift away from longstanding hypotheses, new avenues for diagnosis and treatment are emerging—a number of which converge on the endogenous signaling molecule nitric oxide
Source: Image Created by Audrey Herrald, 2020
Ever since Alois Alzheimer first identified the “peculiar severe disease process of the cerebral cortex” that is now known as Alzheimer’s disease, most efforts to understand and treat the condition have centered upon two concurrent etiologies: extra-neuronal depositions of misfolded protein, known as tau tangles, and intraneuronal buildups of beta-amyloid protein, known as senile plaques (Hippius & Neundörfer, 2003). However, as treatments for Alzheimer’s disease (AD) continue to evade the scientific community, researchers have begun to raise concerns about the validity of these long-accepted pathways for AD pathology (Stefano et al., 2020). While many scientists agree that beta-amyloid aggregation likely contributes to disease onset, growing evidence suggests that these protein plaques are far from the only contributors to the most common form of Alzheimer’s disease (Kametani & Hasegawa, 2018).
In a recent Alzheimer’s disease edition of Scientific American, neurologist Kenneth Kosik situates the problem: “We have not been barking up a completely wrong research tree, but our zeal has led us to ignore other trees and even the roots of this particular one.” Scientists like Kosik suggest that Amyloid beta plaques and tau tangles might be most appropriately regarded as downstream effects of a chronic, whole-body, aging-related state of proinflammation—a theory that could help explain why many drugs that successfully break up Amyloid beta plaques still fail to hinder AD progression (Huang et al., 2020).
So what is this proinflammatory state, and where does nitric oxide come in? When the body is in a proinflammatory state, the immune system becomes hyperactivated. Processes that usually help defend against unwanted viruses and pathogens can become harmful. In the case of Alzheimer’s disease, inflammation contributes to neuronal death by damaging the microvascular networks that supply neurons with oxygen and nutrients (de la Torre & Stefano, 2000). Nitric oxide (NO) is a key signaling molecule in these vascular pathways, helping to mediate the potassium channels that control vascular expansion and constriction (Bolotina et al., 1994). Researchers suggest that carefully controlled NO release in damaged regions of the neural vasculature might improve nutrient and oxygen delivery, thereby slowing neuron death (Stefano et al., 2020). However, the potential therapeutic value of NO is not constrained to neural vasculature; NO can also interact with proteins in the mitochondria to improve metabolic efficiency, essentially helping neurons make the most out of their limited oxygen supply (Cler et al., 2007).
While limited ex-vivo and animal model research supports these findings, certain specifics of NO-related treatment have yet to be clarified (Zhu et al., 2007; Katusic & Austin, 2014; Stefano et al., 2019). Most pressingly, researchers must understand how much NO to release, as well as where in the brain to release it. Sensing experiments suggest that physiologically produced NO can be found in concentrations between ∼100 and 400 nM, diffusing rapidly within an area of about 400 μm before decaying to undetectable levels in a matter of minutes (Ledo et al., 2005). Any potential AD therapy related to NO administration would need to possess good regional specificity (~400 nm diameter) and careful concentration control to avoid the toxic effects of excess NO accumulation, neither of which are trivial feats. However, Kosik and other scientists express optimism that adopting a broader view of AD pathology—one that focuses less on destroying amyloid-beta and tau, and more on systemic, whole-body pathological processes—could be the paradigm shift that will begin to move the needle on Alzheimer’s disease research.
References
de la Torre, J. C., & Stefano, G. B. (2000). Evidence that Alzheimer’s disease is a microvascular disorder: The role of constitutive nitric oxide. Brain Research. Brain Research Reviews, 34(3), 119–136. https://doi.org/10.1016/s0165-0173(00)00043-6
Dementia. (n.d.). Retrieved December 6, 2020, from https://www.who.int/news-room/fact-sheets/detail/dementia
Hippius, H., & Neundörfer, G. (2003). The discovery of Alzheimer’s disease. Dialogues in Clinical Neuroscience, 5(1), 101–108.
Huang, L.-K., Chao, S.-P., & Hu, C.-J. (2020). Clinical trials of new drugs for Alzheimer disease. Journal of Biomedical Science, 27. https://doi.org/10.1186/s12929-019-0609-7
Jin, R. C., & Loscalzo, J. (2010). Vascular nitric oxide: Formation and function. Journal of Blood Medicine, 1, 147–162.
Kametani, F., & Hasegawa, M. (2018). Reconsideration of Amyloid Hypothesis and Tau Hypothesis in Alzheimer’s Disease. Frontiers in Neuroscience, 12. https://doi.org/10.3389/fnins.2018.00025
Scientific American May 2020. (2020). Scientific American, 78.
Stefano, G. B., Esch, T., & Kream, R. M. (2019). Behaviorally-Mediated Entrainment of Whole-Body Metabolic Processes: Conservation and Evolutionary Development of Mitochondrial Respiratory Complexes. Medical Science Monitor : International Medical Journal of Experimental and Clinical Research, 25, 9306–9309. https://doi.org/10.12659/MSM.920174
Stefano, G. B., Esch, T., Ptacek, R., & Kream, R. M. (2020). Dysregulation of Nitric Oxide Signaling in Microglia: Multiple Points of Functional Convergence in the Complex Pathophysiology of Alzheimer Disease. Medical Science Monitor : International Medical Journal of Experimental and Clinical Research, 26, e927739-1-e927739-4. https://doi.org/10.12659/MSM.927739
Zhu, X., Smith, M. A., Honda, K., Aliev, G., Moreira, P. I., Nunomura, A., Casadesus, G., Harris, P. L. R., Siedlak, S. L., & Perry, G. (2007). Vascular oxidative stress in Alzheimer disease. Journal of the Neurological Sciences, 257(1), 240–246. https://doi.org/10.1016/j.jns.2007.01.039
Related Posts
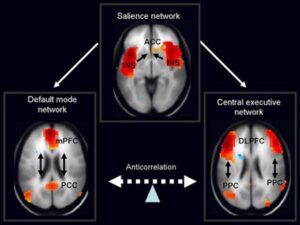
The importance of the Default Mode Network (DMN) in Post-Traumatic Stress Disorder (PTSD)
Figure 1: Neural imaging of the default mode network (pictured...
Read MoreWhy Do We Really Need Vitamins?
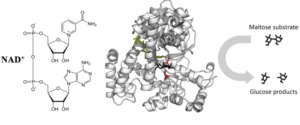
Figure 1: This figure illustrates the interaction between an enzyme,...
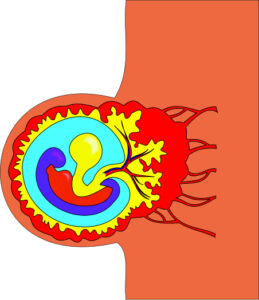
Read MoreEpigenetics: How DNA Gives Birth to Life
Figure 1: Researchers at the Planck Institute for Molecular Genetics...
Read MoreAudrey Herrald

Comments are closed.