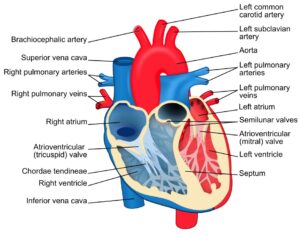
From DNA to Life. (Source: Wikimedia Commons, William Crochot)
Our DNA is like a secret code – 6 billion base pairs (per cell) but only 4 letters, repeated over and over in a seemingly random order. The structure appears relatively simple, but those nitrogenous bases of DNA store the secrets of life, death, evolution, and extinction. Since the Human Genome Project, DNA sequencing studies have received a more public spotlight, and are heralded as the key to solving various human diseases and limitations, ranging from simple baldness to more serious, life-limiting genetic disorders like Huntington’s disease.
Genomic studies are very exciting. However, while the scientific community has been studying human genes, one crucial variable has not received as much attention as it deserves: human variability. People of African and Asian descent are far less represented in genomic research studies than their European counterparts. A recent study, which investigated almost 3000 Genome-Wide Association Studies, showed that 67 percent of the subjects had European ancestry, 29 percent had Asian, and the remaining 4 percent had ancestry from other, underrepresented minorities which were defined as African or African American, Native American, and Hispanic or Latino (Landry et al., 2018). However, Latino Americans make up 18.7% and Black Americans make up 12.1% of US population as of 2020, according to the U.S. Census Bureau (“NPR Cookie Consent and Choices,” 2021). Such racial underrepresentation not only stands to contribute to greater health disparities for marginalized populations but also hinders the progress of genomics by creating gaps in the research.
Modern-day genomic studies investigate different phenotypic and genotypic traits across populations and analyze how a specific gene can give rise to or mitigate certain conditions (McGuire & Gabriel, 2020). These studies may involve comparative research of similarly matched groups (by age, socioeconomic status, etc.) with or without a particular disease at a single point in time. They may also be designed to follow a cohort of individuals through time and see how their genetic profile may predict the onset of certain diseases.
In such studies, considering racial and ethnic differences is imperative. Multiple studies have shown how different races possess distinct genetic predispositions for certain diseases. For example, mutations in the gene encoding beta-globin (HBB), which cause hemoglobin to contort into an abnormal sickle shape and gives rise to sickle cell disease, is more prevalent in people of sub-Saharan African descent (Eridian, 2011). Past studies have shown that the very mutation in HBB that causes sickle cell anemia provides resistance to malaria, which is one of the leading causes of death in Sub-Saharan Africa (Archer et al., 2018). While homozygous recessive individuals with two mutated beta globin alleles develops sickle cell anemia, heterozygous individuals demonstrate resistance to malaria and don’t show significant symptoms of sickle cell disease. This make sense from an evolutionary perspective, given that people of sub-Saharan African descent (and their ancestors) were more likely to have encountered mosquitos carrying the malaria parasite. The existence of malaria provided selective pressure to maintain the mutant HBB gene within the population.
Along similar lines, there is currently a push in field of Cystic Fibrosis (CF) research to study CFTR protein variants (CFTR is the gene that causes CF) in non-white racial/ethnic groups. This push stems from the fact that a smaller proportion of the non-white population is eligible for the recently approved Cystic fibrosis transmembrane conductance regulator (CFTR) modulator drugs, which have been very effective thus far at improving the lung function of people with CF and have the potential to significantly increase life expectancy over time (DiMango et al., 2021).
According to the study by McGarry (2021), CFTR modulator drugs, which target the CFTR protein, are currently approved for people who have 1-2 copies of the most common CF-causing gene variant, known as Delta-F508. This mutation is more common in Caucasians than in Black or Hispanic Americans, which explains why, at least in part, fewer Black and Hispanic Americans are eligible. That is, while over 90% of non-Hispanic White people with CF in the U.S. have CFTR mutations that qualify for the drug, 70% of American Black, 75% of Hispanic, and 80% of other racial minorities with CF have qualifying mutations. This disparity in drug approval has the potential to exacerbate existing disparities in health outcomes for minorities with the disease.
Or take another example. Researchers have identified that having a KRAS mutation in colorectal tumor cells correlates with a decreased response to Cetuximab, a type of chemotherapy drug (Lièvre et al., 2006). A recent study demonstrated that African Americans have a 36% higher rate of mutation in the KRAS gene than Caucasians (Staudacher et al., 2017). This means that African Americans especially are in greater need of new therapeutic options that compensate for Cetuximab resistance.
To better understand these sorts of genomic differences in the human population, assessing how human genes have developed under different environmental pressures is a promising area of research. Since people of various racial and ethnic backgrounds endured distinctive environmental and selective pressures over millennia of time due to differences in ancestry, their genetic response to diverse stimuli and downstream biological effects are bound to be different.
It is not only a matter of studying genomic differences, however. At a higher level, these genomic differences manifest in varied responses to drugs across groups. Underscoring this fact, a recent study identified a significant difference in the ‘molecular signatures’ (i.e., the cell surface proteins of tumor cells) of three different cancer types – colon cancer, non-small cell lung cancer, and high-grade glioma – between African Americans and Caucasians (Heath et al., 2018). In order to understand more precisely how different racial and ethnic groups respond to drugs, clinical trials must become more diverse.
Recent analysis on the participation in cancer clinical trials of people of different racial backgrounds demonstrated a significant underrepresentation of the Hispanic and Black population in studies of certain cancer types (Murthy & Krumholz, 2004). A lack of knowledge of differences in cancer pathology between racial or ethnic groups can lead to greater health disparity where the minorities receive treatment that doesn’t ensure the promised effect, or even worse, not given an option for certain treatment at all because they do not have access to approved drugs.
Since the success of the human genome project, our scientific understanding of human genetics has grown in leaps and bounds. Many scientists are optimistic that further study of human genetics will help unlock the mysteries of diseases that are once thought to be “incurable” – as drugs developed for CF, and sickle cell disease are beginning to do. For example, the new CRISPR technology has shown great promise in treating sickle cell anemia. A recent report has shown that the first treated for sickle cell anemia with CRISPR gene-editing technology in 2019 person (an African American woman from Mississippi named Victoria Gray) continues to be free of symptoms two years on (Stein, 2021). Increasing diversity and inclusion in genetic studies will allow for more stories like this to be told.
References
Annunciata, A. (2008) DNA Packaging: Nucleosomes and Chromatin. Nature Education 1(1):26
Archer, Natasha M et al. (2018). “Resistance to Plasmodium falciparum in sickle cell trait erythrocytes is driven by oxygen-dependent growth inhibition.” PNAS vol .115,28: 7350-7355. doi: ; https://doi.org/10.1073/pnas.1804388115
Bentley, Amy R et al. (2017). “Diversity and inclusion in genomic research: why the uneven progress?.” Journal of community genetics vol. 8,4: 255-266. doi:10.1007/s12687-017-0316-6
DiMango, E., Simpson, K., Menten, E., Keating, C., Fan, W., & Leu, C. S. (2021). Health Disparities among adults cared for at an urban cystic fibrosis program. Orphanet Journal of Rare Diseases, 16(1). https://doi.org/10.1186/s13023-021-01965-4
Erivan, Sandro. (2011). “Sickle cell protection from malaria.” Hematology reports vol. 3,3: e24. doi:10.4081/hr.2011.e24
Heath, Elisabeth I et al. (2018). “Racial Disparities in the Molecular Landscape of Cancer.” Anticancer research vol. 38,4: 2235-2240. doi:10.21873/anticanres.12466
Landry, Latrice G, et al. (2018). “Lack Of Diversity In Genomic Databases Is A Barrier To Translating Precision Medicine Research Into Practice.” Health Affairs, vol. 37, no. 5, doi:10.1377/hlthaff.2017.1595 HEALTH AFFAIRS 37, NO. 5 (2018): 780–785.
Lièvre, Astrid et al. (2006). “KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer.” Cancer research vol. 66,8: 3992-5. doi:10.1158/0008-5472.CAN-06-0191
McGarry, M. E., Gibb, E. R., Oates, G. R., & Schechter, M. S. (2021). Left Behind: The Potential Impact of CFTR Modulators on Racial and Ethnic Disparities in Cystic Fibrosis. Paediatric Respiratory Reviews. https://doi.org/10.1016/j.prrv.2021.12.001
McGuire, A.L., Gabriel, S. (2020), Tishkoff, S.A. et al. The road ahead in genetics and genomics. Nat Rev Genet 21, 581–596. https://doi.org/10.1038/s41576-020-0272-6
Murthy VH, Krumholz HM, Gross CP. Participation in Cancer Clinical Trials: Race-, Sex-, and Age-Based Disparities. JAMA. 2004;291(22):2720–2726. doi:10.1001/jama.291.22.272
NPR Cookie Consent and Choices. (2021, August 13). NPR. https://choice.npr.org/index.html?origin=https://www.npr.org/2021/08/13/1014710483/2020-census-data-us-race-ethnicity-diversity
Staudacher, J. J., Yazici, C., Bul, V., Zeidan, J., Khalid, A., Xia, Y., Krett, N., & Jung, B. (2017).
Increased Frequency of KRAS Mutations in African Americans Compared with Caucasians in Sporadic Colorectal Cancer. Clinical and translational gastroenterology, 8(10), e124. https://doi.org/10.1038/ctg.2017.48
Stein, Rob. (2021) “First Sickle Cell Patient treated with CRISPR gene-editing still thriving”. NPR
Related Posts
Covid-19 and the Next Pandemic: Designing a Science-based Strategy to Prepare for the Next Pandemic
Taking the proper, science-backed steps could help prevent the next...
Read MoreThe H.U.N.G.E.R. Initiative (Helping Underserved Neighborhoods Generate Equitable Resources)
This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023...
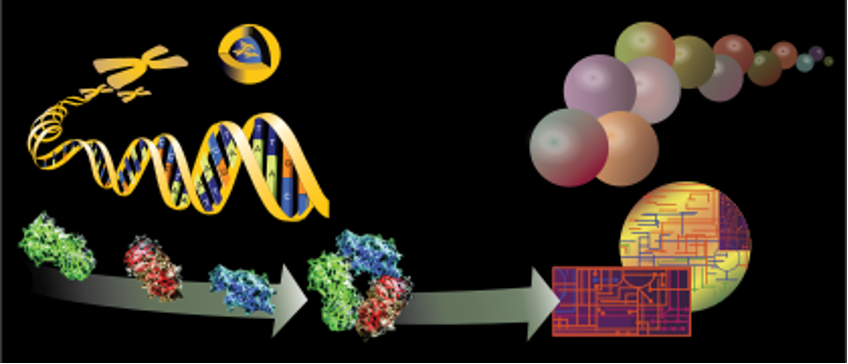
Read MoreAn International Team of Researchers Just Solved One of the Biggest Mysteries About the Human Heart
Figure 1: The heart is one of the most complex...
Read MoreVirtual Reality as a Rehabilitation Technology
Figure 1: A veteran makes use of the Computer Assisted...
Read MoreThe Critical Role of Sleep in Determining Reaction to Daily Life
Source: Pixabay Sleep plays an extremely important role in physical...
Read MoreThe Importance of Model Organisms
Many important discoveries in human biology that affect how we...
Read MoreJY