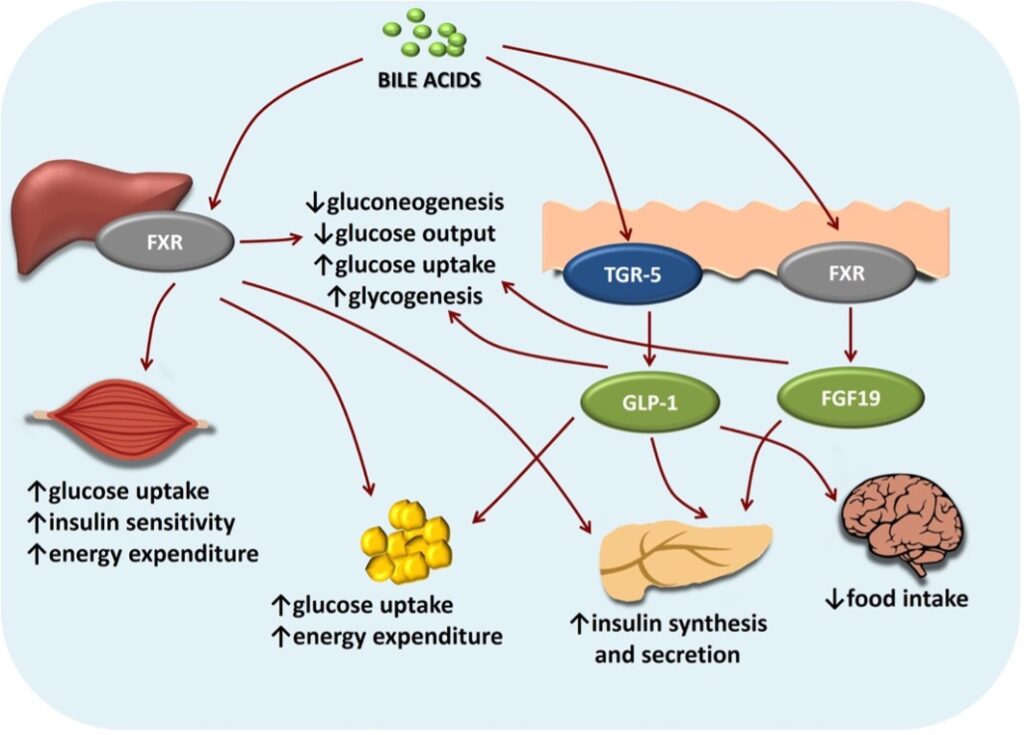
Figure 1: Diagram of the effects of bile acids on food intake. Bile acids from the digestive system bind to TGR-5 receptors on the surface of hypothalamic cells in the brain to effectively increase insulin synthesis and decrease food intake
Source: Frontiers, Danic et al.
Obesity has become a worldwide health crisis affecting approximately 13% of the global population, with dangerous health implications including heart disease and diabetes. Prescription medications, such as Lorcaserin, are effective in promoting weight loss by acting directly on serotonin receptors in the brain to cause earlier satiety (fullness). However, these medications are associated with extremely harmful side effects, such as suicidal thoughts, increased occurrence of cancers, and birth defects (Kushner, 2014). Additionally, CDC estimates from the years 2013-2016 indicate that 89% of US adults diagnosed with diabetes are also obese or overweight (National Diabetes Statistics Report, 2020). Type 2 diabetes is characterized by insulin resistance and inadequate insulin secretion (Diabetes – Symptoms and Causes, 2020). For these reasons, there is a high demand for research into safer medications that can manipulate hunger/satiety pathways to decrease food intake.
The body’s system for regulating food intake is mainly controlled by the hypothalamus, a structure in the brain which is responsible for maintaining the steady state of systems in the body, called homeostasis. The widely accepted theory as to how the stomach conveys hunger and satiety signals to the brain involves special types of neurons in the hypothalamus – the NPY/AgRP neurons – which act to increase appetite and also decrease energy expenditure. The chain of events that leads to increased appetite, and ultimately more eating, actually starts in the stomach, where low nutrient availability causes the release of hormones, such as ghrelin, that can bypass the blood brain barrier through leaky blood vessels in the hypothalamus and bind to NPY/AgRP neurons (Proietto, 2015).
This model of satiety has stood for a long time. Recently, however, researchers at Schoonjan’s lab at Ecole Polytechnique Féderale de Lausanne (EPFL) identified a link between bile acids and satiety that could add to our understanding of how nutrient availability information is conveyed.
Bile acids are the most abundant metabolites in the gut. They help the body digest food and absorb fat-soluble vitamins. During a meal, the gallbladder deposits bile into the gut to increase lipid surface area, augment absorption, and aid with digestion (Chen, 2021). And as the researchers in Schoonjan’s lab have found, bile acids also act as a key relay messenger of nutrient availability. After leaving the digestive tract, bile acids temporarily enter the bloodstream and then accumulate in the hypothalamus where they bind to G-protein-coupled bile receptors (TGR-5) on the surface of NPY/AgRP neurons (Ecole Polytechnique Fédérale de Lausanne, 2021). The binding of bile acids to this receptor produces both short-term blocking of AgRP/NPY peptide release and a long-term inhibition of their expression (Ecole Polytechnique Fédérale de Lausanne, 2021). Considering that NPY/AgRP neurons produce hunger signals, the ability of bile acids to inhibit these signals will suppress hunger and consequently may be used at appropriate doses to combat obesity.
To demonstrate the efficacy of bile acids as a potential obesity treatment, Schoonjan’s lab induced obesity in mice with high-fat diets and measured the effects of TGR-5 activation. Their study demonstrated the ability of bile acids to activate TGR-5 and successfully attenuate obesity in diet-induced obese mice models (Ecole Polytechnique Fédérale de Lausanne, 2021). Therefore, the bile acid-TGR-5 axis provides a promising future for obesity and type 2 diabetes treatments by inhibiting expression of hunger signals induced by NPY/AgRP neurons.
References
Chen, I. (2021). Physiology, Bile Acids. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK549765/.
Diabetes – Symptoms and causes. (2020). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
Ecole Polytechnique Fédérale de Lausanne. (2021). Bile acids trigger satiety in the brain. ScienceDaily. Retrieved May 31, 2021 from www.sciencedaily.com/releases/2021/05/210524161743.htm
Guo, C., Chen, W. D., & Wang, Y. D. (2016). TGR5, Not Only a Metabolic Regulator. Frontiers in physiology, 7, 646. https://doi.org/10.3389/fphys.2016.00646
Proietto, J. (2015). Chemical messengers: How hormones make us feel hungry and full. The Conversation. https://theconversation.com/chemical-messengers-how-hormones-make-us-feel-hungry-and-full-35545#:~:text=Ghrelin%20is%20made%20in%20the,the%20release%20of%20ghrelin%20increases.
Kushner, R. F. (2014). Weight loss strategies for treatment of obesity. Progress in cardiovascular diseases, 56(4), 465-472.
Perino, A., Velázquez-Villegas, L.A., Bresciani, N. et al. (2021). Central anorexigenic actions of bile acids are mediated by TGR5. Nat Metab 3, 595–603. https://doi.org/10.1038/s42255-021-00398-4
U.S. Dept of Health and Human Services. (2020). (rep.). National Diabetes Statistics Report, 2020. Atlanta, GA.
Related Posts
An Overview of Oncology Treatments
Lead Authors: Dina Rabadi1, Sarah Matatov2 Co-Authors: Carolina Guerrero1, Nina...
Read MoreStudy Finds Anthrax Toxin as Possible Substitute for Painkillers
Figure: A computer representation of the anthrax toxin protein (Source:...
Read MoreFighting Hospital Hardships: An Intervention for Reducing Stress in Hospital Workers
Figure 1: This figure describes some of the symptoms of...
Read MoreIsabelle Wilson