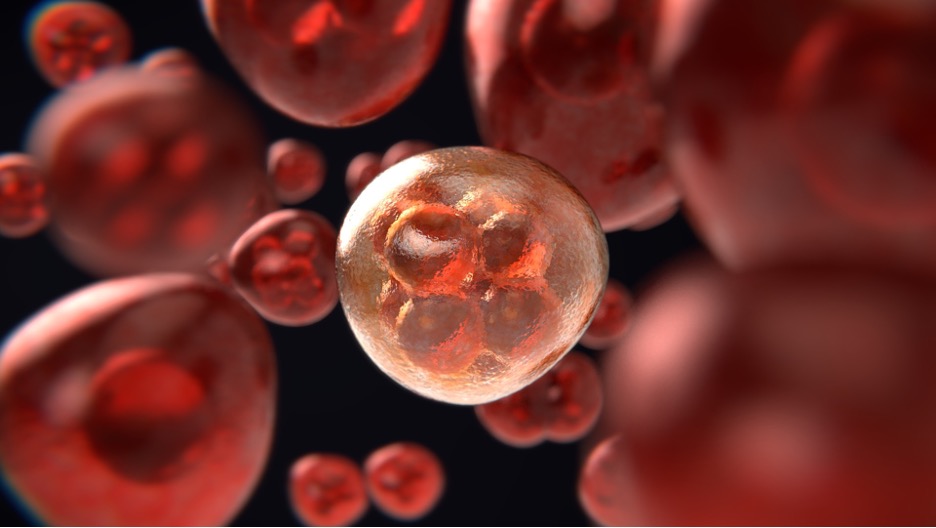
Figure: Cancer cell division is rapid and uncontrollable. New evidence suggests that the gut microbiome may contribute to cancer cell proliferation, spurred on by a high fat diet – but also that there may be ways to fix a cancer-causing gut microbiome (Source: Pixabay, ColiN00B)
Background
The war on cancer has been fought valiantly for decades – with billions of dollars spent on drugs that extend lives. In this war, great battles have been won, with a wealth of new treatments and a large drop in the cancer death rate – down more than 25% – since the declaration of the War on Cancer in 1971. Yet the war still rages on. For some cancers like colorectal cancer (CRC), currently the 3rd most diagnosed cancer worldwide, case numbers are still quite high (even though they have been decreasing steadily over the past few decades). Given the current rate of CRC in the US population, about 150,000 US adults are expected to be diagnosed this year. But there is hope that many current and future CRC patients may find salvation from an unlikely source – the bacteria living in their gut.
Details
Why would gut bacteria effect the development of cancer? For one, CRC develops in the large intestine, meaning that gut microbes live in close proximity to cancerous tissue as it grows – able to receive chemical signals from cancer cells and send chemical signals back. Scientists also know that a high fat diet is a risk factor for colorectal cancer (as it is for many other conditions, like obesity and type II diabetes). The gut microbiome helps break down complex dietary nutrients – thus, its composition and activity are heavily influenced by an individual’s diet. Knowing all this, scientists working out of the Chinese University of Hong Kong took the next logical step and decided to investigate how the microbes in the gut, influenced by a high fat diet, might be contributing to cancer.
It is already well-known that the gut microbiome community tends to be altered in the early stages of colorectal cancer. But the research team wanted to know in greater detail how a high fat diet specifically affects the members of the gut microbiome and their chemical products (metabolites) – and how the activity of the gut microbiome might be a risk factor for CRC. To accomplish this, they turned to trusty mice models, sacrificed for the greater good of human cancer patients. The mice used by the research team were special, having an in-born tendency to develop pancreatic cancer, so the researchers knew they would develop tumors at some point over the course of the experiment. To confirm their hypothesis that mice given a high-fat diet are more prone to CRC, they just needed to show that high fat diet mice developed CRC at a greater rate than those which were given a control diet lower in fat.
As hypothesized, the researchers found that the mice given the high fat diet indeed developed more colorectal tumors at a greater volume. They then looked at the microbiome more closely, and here too found distinct differences. Mice given the high fat diet had an elevated abundance of certain pathogenic species (namely those of the genus Allistipes), and a lower abundance of certain probiotic species (specifically, Parabacteroides distasnosis). Furthermore, the high fat diet mice exhibited elevated levels of the compound lysophosphatidic acid, a metabolite generated by bacteria.
The researchers wanted to further confirm that elevated cancer risk in high fat diet mice was due to changes in the microbiome. So, they brought another mouse model into play: the germ free mouse. These mice are quite useful as a research tool because their gut is free of micro-organisms – therefore, scientists can transplant bacteria from the gut of the CRC mice into the germ-free mice and observe their direct effect. Such an experiment would tell the researchers whether it is the microbes themselves – and not some other factor in the guts of mice with CRC – that is driving cancer development. Transplanting bacteria from the CRC mice to the germ-free mice did lead to cancerous growth in the germ-free mice, suggesting that the microbes themselves are responsible
Takeaways
With knowledge of the role that the gut microbiome plays in CRC, scientists may be able to come up with new methods to treat cancer. Given that the gut microbiome tends to be altered at very early stages of colon cancer, if these changes can be identified early on they might be reversed before cancer spreads throughout the body and becomes highly fatal. This present study helps scientists and drug developers understand what options they have to reverse negative changes in the gut microbiome. They could try to eliminate certain pathogenic bacteria or bring back in probiotic bacteria so the gut microbial community returns to normal. Targeting the metabolites overproduced by the microbiome in CRC cases may also help stop the microbiome from promoting cancerous growth.
References
Featured Article:
Yang, J., Wei, H., Zhou, Y., Szeto, C. H., Li, C., Lin, Y., Coker, O. O., Lau, H., Chan, A., Sung, J., & Yu, J. (2022). High-Fat Diet Promotes Colorectal Tumorigenesis Through Modulating Gut Microbiota and Metabolites. Gastroenterology, 162(1), 135–149.e2. https://doi.org/10.1053/j.gastro.2021.08.041
Other Sources:
Biosciences, T. (n.d.). What Are Germ-Free Mice and How Are They Sourced? Retrieved May 8, 2022, from https://www.taconic.com/taconic-insights/microbiome-and-germ-free/what-are-germ-free-mice.html
Boston, 677 Huntington Avenue, & Ma 02115 +1495‑1000. (2017, August 16). The Microbiome. The Nutrition Source. https://www.hsph.harvard.edu/nutritionsource/microbiome/
Colorectal Cancer—Statistics. (2012, June 25). Cancer.Net. https://www.cancer.net/cancer-types/colorectal-cancer/statistics
DeVita, V. T. (2004). The “War on Cancer” and its impact. Nature Clinical Practice Oncology, 1(2), 55–55. https://doi.org/10.1038/ncponc0036
Harrar, S. (n.d.). As the War on Cancer Turns 50, Treatments Are Improving. AARP. Retrieved May 8, 2022, from https://www.aarp.org/health/conditions-treatments/info-2021/cancer-progress.html
Yu, J., Feng, Q., Wong, S. H., Zhang, D., Liang, Q. yi, Qin, Y., Tang, L., Zhao, H., Stenvang, J., Li, Y., Wang, X., Xu, X., Chen, N., Wu, W. K. K., Al-Aama, J., Nielsen, H. J., Kiilerich, P., Jensen, B. A. H., Yau, T. O., … Wang, J. (2017). Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut, 66(1), 70–78. https://doi.org/10.1136/gutjnl-2015-309800
Related Posts
Intergenerational Trauma: How a history of pain brings biological costs
Source: Nicolas Raymond, CC BY 2.0 A few years ago,...
Read MoreModeling Maximum Running Speed in Animals
Figure: Two cheetahs lie side by side. As the fastest...
Read MoreGenetic Cheating? Identifying CRISPR/Cas Gene Doping
Figure 1: Lance Armstrong, a well-known professional cyclist, has been...
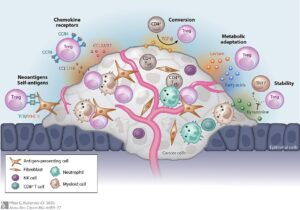
Read MoreRegulating Regulatory T Cells to Fight Cancer
Figure 1: The different ways a tumor can provide protection...
Read MoreAn Overview of Oncology Treatments
Lead Authors: Dina Rabadi1, Sarah Matatov2 Co-Authors: Carolina Guerrero1, Nina...
Read MoreOverview, History, Essential Concepts, and Current Topics in Transplant Immunology
First Author: Anahita Kodali1 Co-Authors: Vaishavi Agrawal2, Vivek Babu3, Sakeena...
Read MoreSam Neff