This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023 Summer Program.

Source: Hush Naidoo Jade Photography
Abstract
Background: Health literacy is the ability of an individual to find, understand, and use health-related services and information to maneuver the complex healthcare system in the U.S., and to advocate for themselves and their own health.
Objective: The purpose of this literature review is to analyze health literacy in the U.S. population and the determinants that lead to low health literacy rates. By understanding these factors, the current health interventions promoting health literacy awareness, and any possible future intervention programs can be better devised to improve health literacy in the U.S.
Methods: This literature review was conducted with scholarly sources from Google Scholar and PubMed, relevant to the keywords.
Results: Through analysis of various determinants of health, minority populations seem to be affected the most by low health literacy rates, especially due to factors such as low education levels, low socioeconomic status, cultural differences, language barriers, and insufficient community resources.
Conclusions: To combat the determinants that contribute to low health literacy, awareness must be created to increase literacy rates. Targeted interventions for the specific demographics most affected must also be implemented to overall promote health equity.
Keywords: Health Literacy, Miscommunication in Healthcare, United States, Social Determinants of Health, Health Interventions, Health Implications, Epidemiology
Introduction
Health literacy is the extent to which a person can access health related information and apply this information to their health-related behaviors. Health literacy is a necessary skill to ensure quality of life by helping shape and improve one’s health, while at the same time promoting health equity among all. Unfortunately, only 12% of the U.S. population is properly health literate to efficiently navigate the healthcare system. Because of this, low health literacy is a major factor for increased healthcare burden on individuals, leading to a higher chance of various conditions and increasing the risk of death for the health illiterate population. Lack of health literacy results in difficulty in refilling prescription medications, processing medicine labels, understanding the right dose, and taking medications at the right time. Furthermore, low health literacy costs the U.S. economy up to $238 billion annually, placing a strain on the healthcare system, as resources are overspent continuously on repetitive problems that can be solved with less effort in a more health literate and health aware system. The issue of low health literacy in the U.S. must be addressed by increasing health education for all, in order to reduce any worsened health outcomes in the U.S caused by low health literacy7.
Epidemiology
Health literacy affects a huge percentage of the US population. 88% of US adults have substandard rates of health literacy, with 14% having below basic knowledge, 22% having basic knowledge, and 55% having intermediate knowledge of health information. This is a significant number of people, and steps must be taken to increase health literacy rates in the US15.
Health literacy rates also differ by certain demographics. The older population, namely those 65 years or older, have the lowest levels of health literacy. In general, trends show that health literacy rates decline after the age of 40. These trends can be attributed to general decreases in cognitive ability in those of older ages, as well as unfamiliarity with digital tools currently used in the healthcare system. However, studies have shown that there is no significant difference in health literacy rates between men and women. By race, Hispanic and African American populations have the lowest health literacy rates, while White and Asian American/Pacific Islander populations have the highest health literacy rates. Also, health status correlates with health literacy, as 42% of those who reported poor health have below basic knowledge of health literacy15.
Social Determinants of Health
Social Determinants of Health (SDOH) are uncontrollable conditions or factors that affect an individual which can impact their health and, in this case, health literacy rates. There are various determinants that affect a person’s health literacy knowledge in the US, including socioeconomic status, such as income and occupational status, education levels, cultural traditions, language, and community8.
Education
Education is perhaps one of the most important SDOH affecting health literacy. Many studies have found that the health literacy of an individual has a direct correlation to their level of education4. This is because education allows an individual to have an increased number of skills that can aid in understanding complex situations, such as navigating the healthcare system. In addition, higher education levels offer an individual more opportunities for success, which in turn increases their quality of life through higher income, better living conditions, and overall higher socioeconomic status relative to an individual who is less educated23.
Socioeconomic Status
As mentioned previously, higher educational qualifications tend to lead to a higher socioeconomic status, relating to wages and employment status, which is directly linked to increased health literacy and health promoting behaviors16. Increased wages allows greater access to quality healthcare resources and treatments, as well as better living conditions, all of which promote health literacy. Moreover, an improved employment status can increase access to social resources and influence, which once again creates easier accessibility to different resources that can enhance health literacy20. However, those with lower socioeconomic status, namely minority populations who on average receive lower wages and older adults who are less likely to be employed, are faced with inadequate resources and health literacy, increasing health implications25.
Culture
Cultural beliefs are one of the key reasons that health literacy rates are low among certain minority populations. Cultural beliefs dictate various behaviors and practices, such as situations in which individuals seek treatment and from whom, as well as perspectives on various health problems11. For example, a certain health condition may be stigmatized in a certain culture, leading to an individual refusing to seek medical attention for the condition. Not only that, patient-provider communication can be greatly influenced by differing cultural beliefs, which can be less inclusive of certain cultures and may also decrease quality of care. One study found that African American individuals experience less patient centric visits, and patient-provider visits are often much shorter than those with White individuals, primarily due to less inclusive cultural environments in many healthcare interactions that can lead to less tailored and less informative care. Cultural barriers to health literacy are enhanced further by language differences14.
Language
Language is an SDOH that stems from culture to affect health literacy rates. A large number of people in the United States have limited English proficiency; specifically, 21.6% of US residents don’t speak English at home. This affects their knowledge, awareness, and decisions within the healthcare system. This is mainly due to decreased communication ability with healthcare providers, which would mean that those who are not proficient in English will be less informed of their health condition and treatment options available14. Furthermore, differences in languages prohibit individuals from inquiring further about their conditions, which could leave them misinformed with regards to caring for themselves. Moreover, a lack of English fluency also affects a person’s ability to understand medication instructions, health education pamphlets, consent forms, and bills, as well as fill out forms at clinics, insurance claims, and more. Overall, language is a major barrier in health literacy levels22.
Community
An individual’s neighborhood and living environment can also affect their health literacy. While some neighborhoods have a plethora of resources available for individuals, such as hospitals, specialized clinics, educational centers, and safe spaces, other communities lack these. This in turn influences the medical services and reliable treatment options available for individuals living in these communities. Moreover, if an entire community’s health literacy rates are low, they may depend on questionable networks and sources of information, which may harm their health. For example, there could be certain stigmas embedded within a certain group in a community that could discourage individuals from seeking care as they are influenced by their community’s beliefs3.
Health Implications
Low health literacy is directly linked to poorer health outcomes, as it is key in preventing and controlling any health conditions. Those who are not health literate may not understand health education materials and are less likely to get tested for any health conditions, preventing early diagnosis and treatment of various conditions, ultimately leading to worsened states of health. This is why low health literacy is often linked with obesity, poor nutrition, and lack of frequent exercise8. Those who are not health literate have, on average, a 50% higher chance of hospitalization, with hospital stays longer by two days on average, and health care costs that are four times higher than for individuals who are health literate19. Moreover, those who are less health literate have a higher probability of frequenting the emergency room within 90 days of being discharged from a hospital21. Also, individuals who have low health literacy are more likely to have comorbidities such as diabetes and hypertension, and are less likely to follow treatment plans or adhere to medication. Ultimately, these all lead to increased chances of mortality from various health conditions for the health illiterate population of the United States13.
Challenges
There are many challenges involved with distributing health literacy to all in the United States. Barriers involved with communication, shame, and quality schooling all tend to affect health literacy. Because the U.S. is filled with a diverse range of cultures, these challenges tied with racism and prejudice combine to become disadvantageous in certain communities, making health literacy inadequate in many populations.
Low Quality Education
Health literacy curriculums in schools are usually designed to assist students in grades 9 through 12 to identify and use reputable sources of high-quality health information, by describing how various sources influence personal health behaviors to teach the process of finding, understanding, and utilizing health-related materials. Quality education must be provided to high school students, and even children at young ages, to help teach how to prevent health problems and better manage health issues when they arise. Poor and inadequate education of health literacy from the start of a young to teenage age can lead to students being to be unfamiliar with medical terms or how their bodies work when they start to age. Due to this, usual patient education materials in hospitals and clinics have been suggested to be written at a sixth-grade or lower reading level, preferably including illustrations, for optimal comprehension of health literacy5.
These are some of the largest barriers to improving understanding health literacy for individuals in the United States. Language barriers cause miscommunications with treating health, low-literacy stigma prevents individuals from reaching out to for much-needed medical care, and low-quality education justifies corresponds to why individuals in the U.S. have low knowledge on health literacy. To address these challenges, measures must be taken to ensure rising health literacy rates in the U.S.6
Language
Because the U.S. is filled with numerous immigrants from various countries, many individuals cannot understand, speak, read, or write in English. In fact, about 22% of individuals in the US do not speak English as their first language. Nevertheless, the U.S. uses English in many informational services like government, education, and commerce. This is very disadvantageous for immigrants or individuals who cannot understand the language that is used to disseminate health information, interpret medical charts, and utilize medical tools for personal and familial healthcare2. It has been found that language barriers in healthcare may lead to miscommunication between a medical professional and patient, reducing both parties’ satisfaction and decreasing the quality of healthcare delivery and patient safety. Misunderstandings may occur in clinical situations in almost half of all healthcare interactions. Poor communication between clinicians and patients can result in misunderstandings about medications and miscommunication about follow-up instructions, resulting in the possibility of poorer outcomes. However, it has been suggested that implementing online translation tools may improve the efficiency of healthcare and the level of satisfaction among both medical providers and patients1.
Stigma
Stigma surrounding low health literacy refers to the shame caused by others or perceived by patients that is associated with the discovery of an individual’s low literacy ability. Low-literacy-related stigma can seriously diminish individuals’ spoken interactions with healthcare professionals and their potential to benefit from healthcare services, ultimately leading to poorer health outcomes, such as unsafe or inappropriate use of medications and a decreased use of preventive healthcare services24. Many patients do not feel at ease with their low health literacy levels, usually due to facing previous humiliation and degradation, preventing them from reaching out to much-needed medical providers. Health professionals must provide non-judgmental literacy-sensitive support and use simple terminology for patients to feel more comfortable with their literacy level and to promote positive healthcare experiences and outcomes9.
Existing Interventions
The issue of health literacy can be addressed through various means. For example, health literacy can be spread not only through written methods, such as various brochures and pamphlets, but also by increasing general literacy and reading ability. Interventions can also include educational workshops that target various cultures and demographics. Technology can be leveraged to create a mass media health literacy awareness campaign, or to publish resources such as articles and videos in an accessible manner. Patient-provider communication is key as well, so interventions could educate doctors, nurses, and other professionals on how to assess whether a patient has low health literacy, and how to efficiently communicate with them to inform them about various health implications and treatments17.
Across the United States, there are various initiatives that target health literacy. Over 20 states have organizations that specifically improve health literacy among the population, such as the Colorado Health Literacy Coalition and the North Carolina Program on Health Literacy. Moreover, various universities, specifically through their public health programs, create resources and tools for individuals to improve their health literacy. Finally, federal initiatives, such as the Affordable Care Act and the Plain Writing Act, improve health literacy rates in the United States12.
One such federal initiative is the National Action Plan to Improve Health Literacy. The plan’s goals are to ensure health information and health equity for all by promoting the communication of health information in an accessible way. It involves key improvements to the healthcare system. These improvements include a set standards to assess health literacy, adequate resources for increased health literacy, and more thorough health education in schools and universities. The plan also involves the promotion of organizations and campaigns that increase health literacy access18.
There are various tools available for assessing health literacy. For example, the Rapid Estimate of Adult Literacy in Medicine, Short Form, or REALM-SF, is a short test containing 7 words. The test asks individuals whether they recognize each word or not, and it is a quick method for healthcare providers to assess a patient’s health literacy. Another test is the Test of Functional Health Literacy in Adults, or TOFHLA Numeracy, which assesses whether a patient can adhere to health care provider instructions. Overall, these tests are useful resources for healthcare providers to determine the best methods of communication to employ with a patient10.
Conclusion
Overall, increased health literacy is necessary in the United States to improve health outcomes, especially in certain minority demographics and populations. Although there are currently many health interventions addressing the urgent issue of health literacy, there are some challenges that these interventions have yet to address, such as the stigma associated with some interventions, or even other determinants such as discrimination and culture. Ultimately, a wider range of targeted interventions must be designed to improve health literacy in the United States and eliminate its burden on the national population.
References
- Alder, S. (2020). Effects of Poor Communication in Healthcare. HIPAA Journal https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/
- Al Shamsi, H., Almutairi, A. G., Al Mashrafi, S. & Al Kalbani, T. (2020). Implications of Language Barriers for Healthcare: A Systematic Review. Oman Med. J. 35, e122
- Alumni Community. Community health literacy model. https://sph.umd.edu/research-impact/research-centers/horowitz-center-health-literacy/projects/health-departments-and-community-coalitions/community-health-literacy-model
- Bayati, T., Dehghan, A., Bonyadi, F. & Bazrafkan, L. (2018). Investigating the effect of education on health literacy and its relation to health-promoting behaviors in health center. J. Educ. Health Promot. 7, 127
- CDC. (2022). Schools. Centers for Disease Control and Prevention https://www.cdc.gov/healthliteracy/education-support/schools.html
- CDC. (2023). Understanding health literacy. Centers for Disease Control and Prevention https://www.cdc.gov/healthliteracy/learn/Understanding.html
- CDC. (2023). What is health literacy? Centers for Disease Control and Prevention https://www.cdc.gov/healthliteracy/learn/index.html
- Coughlin, S. S., Vernon, M., Hatzigeorgiou, C. & George, V. (2020). Health Literacy, Social Determinants of Health, and Disease Prevention and Control. J Environ Health Sci 6
- Easton, P., Entwistle, V. A. & Williams, B. (2013). How the stigma of low literacy can impair patient-professional spoken interactions and affect health: insights from a qualitative investigation. BMC Health Serv. Res. 13, 319
- Guides: Health literacy resources: Assessment. (2009)
- Health literacy fact sheets. (2013). Center for Health Care Strategies https://www.chcs.org/resource/health-literacy-fact-sheets/
- Health literacy interventions. County Health Rankings & Roadmaps https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/strategies/health-literacy-interventions
- Hickey, K. T. et al. (2018). Low health literacy: Implications for managing cardiac patients in practice. Nurse Pract. 43, 49–55
- Institute of Medicine (US) Committee on Health Literacy, Nielsen-Bohlman, L., Panzer, A. M. & Kindig, D. A. Culture and Society. (National Academies Press (US), 2004).
- Kim, B. & Sacks, K. Health literacy in the United States: Enhancing assessments and reducing disparities. Milken Institute https://milkeninstitute.org/report/health-literacy-us-assessments-disparities
- Ma, T. et al. (2021). Health Literacy Mediates the Association Between Socioeconomic Status and Productive Aging Among Elderly Chinese Adults in a Newly Urbanized Community. Front Public Health 9, 647230
- Meherali, S., Punjani, N. S. & Mevawala, A. (2020). Health Literacy Interventions to Improve Health Outcomes in Low- and Middle-Income Countries. Health Lit Res Pract 4, e251–e266
- National action plan to improve health literacy. (2018). https://health.gov/our-work/national-health-initiatives/health-literacy/national-action-plan-improve-health-literacy
- Research guides: Health literacy: Impact of health literacy.
- Rikard, R. V., Thompson, M. S., McKinney, J. & Beauchamp, A. (2016). Examining health literacy disparities in the United States: a third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health 16, 975
- Shahid, R. et al. (2022). Impact of low health literacy on patients’ health outcomes: a multicenter cohort study. BMC Health Serv. Res. 22, 1148
- Singleton, K. & Krause, E. M. S. (2010). Understanding cultural and linguistic barriers to health literacy. Ky. Nurse 58, 4, 6–9
- Social determinant of health: Education is crucial. School of Public Health https://publichealth.tulane.edu/blog/social-determinant-of-health-education-is-crucial/ (2021)
- Stigma of low health literacy. https://www.ruralhealthinfo.org/toolkits/health-literacy/4/stigma
- Svendsen, M. T. et al. (2020). Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health 20, 565
Related Posts
The E.C.H.O. Initiative: Encouraging Cardiovascular Health Through Outreach
This publication is in proud partnership with Project UNITY’s Catalyst Academy 2023...
Read MoreDancing Neurons & Their Exciting Impacts
Figure 1: A network of neurons in the brain Source: Elizabeth...
Read MoreThermophilic Life in Yellowstone National Park Challenges the Physical and Chemical Limits of Survival
Cover Image: Grand Prismatic Spring in Yellowstone National Park (Source:...
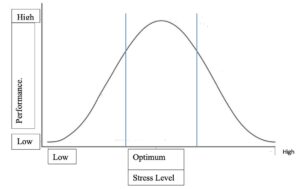
Read MoreRetitling Stress: A Look at the Yerkes-Dodson Law
Figure 1: This graph compares stress level with performance at...
Read MoreUnderstanding the Social Factors Affecting Cancer Therapy
Cover Image: A patient being prepared for radiation therapy. (Source:...
Read MoreEarly Childhood Adversity Impacts Impulsive Decision-Making
Cover Image: An image of a girl holding a stuffed...
Read MoreDipikkasri Dhananjeyan, Smriti Kumar